Hyperthyroidism
Find your care
We deliver effective, minimally invasive treatments in a caring environment. Call 310-267-7838 to connect with an expert in endocrine surgery.
Hyperthyroidism (overactive thyroid)
UCLA treats hyperthyroidism (an overactive thyroid) with expert care using medication, surgery, and radioactive iodine.
Hyperthyroidism FAQs
What is Hyperthyroidism?
Hyperthyroidism is a condition describing the overproduction of thyroid hormone from the thyroid gland.
What are Signs and Symptoms Hyperthyroidism?
Symptoms are different for each person.
Here are the most common ones:
- Nervousness
- Irritability
- Sweating more than normal
- Thinning of the skin
- Fine, brittle hair
- Weak muscles, especially in the upper arms and thighs
- Shaky hands
- Fast heartbeat (palpitations)
- High blood pressure
- More bowel movements than normal, diarrhea
- Weight loss
- Trouble dealing with the heat
- Problems sleeping
- Prominent eyes
- Sensitivity to bright light
- Confusion
- Irregular menstrual cycle in women
- Tiredness and lack of energy (fatigue)
- Larger than normal thyroid gland (goiter)
How is Hyperthyroidism Diagnosed?
At the UCLA Endocrine Center, you will meet with an endocrinologist who will ask about your past health, including your medications and diet, and perform a comprehensive physical exam.
Blood tests can help diagnose hyperthyroidism. Laboratory tests to determine thyroid function include:
- Thyroid Stimulating Hormone (aka TSH) helps indicate whether the thyroid is working correctly
- Measurements of the two forms of thyroid hormone, T4 and T3
- If indicated, measurements of specific antibodies targeted to the thyroid and its receptors
The workup may also include neck ultrasound to assess for thyroid nodules that could be overproducing thyroid hormone.
What Causes Hyperthyroidism?
Hyperthyroidism has several causes. These may include:
Graves’ disease
Graves’ disease is the most common form of hyperthyroidism (an overactive thyroid gland) in the U.S. and worldwide. It is an autoimmune disease, in which the immune system stimulates the thyroid to overproduce thyroid hormones. In addition to symptoms of hyperthyroidism, Graves’ disease can be associated with thyroid eye disease symptoms, such as swelling, redness, and bulging of the eyes.
How is Hyperthyroidism Treated?
Treatment will depend on your symptoms, age, and general health. It will also depend on how severe the condition is.
Treatment may include:
- Medicine. It can help lower the level of thyroid hormones in the blood.
- Radioactive iodine. It comes in the form of a pill or liquid. It slowly destroys the cells of the thyroid gland so that less thyroid hormone is made.
- Surgery. You may need to have all or part of your thyroid removed.
- Beta blockers. These medicines block the action of the thyroid hormone on the body. That helps with rapid heart rate and palpitations.
What are Possible Complications of Hyperthyroidism?
If your hyperthyroidism is not treated, these complications may happen:
- Thyroid crisis, when symptoms get worse because of stress or illness
- Heart problems, such as an abnormal rhythm or heart failure
- Weak, brittle bones (osteoporosis)
- Pregnancy problems, such as miscarriage, early delivery, and preeclampsia or high blood pressure
Preparation Before Surgery
Toxic solitary nodule or multinodular goiter
These can be treated with radioactive iodine or surgery. For patients who refuse both, patients can be given long-term thionamides. Surgery is recommended for toxic nodules or multinodular goiters when:
- Presence of large goiter
- Patient has compressive symptoms
- Patient also has thyroid malignancy
- Patients who do not desire radioactive iodine
Large Goiters
Any enlargement of the thyroid gland is referred to as a “goiter.” Goiter can be caused by Hashimoto’s Thyroiditis (an autoimmune disease) and iodine deficiency. These do not require treatment unless the goiter is causing compressive or hyperthyroid symptoms.
Thyroiditis
This is a general term that refers to inflammation of the thyroid. Depending on the severity, thyroiditis may or may not produce any symptoms or need to be treated. The inflammation releases an excessive amount of thyroid hormone, leading to temporary hyperthyroidism. As the thyroid “burns out,” the thyroid then often becomes underactive.
Less common causes of hyperthyroidism include:
- Taking too much thyroid hormone medicine to treat an underactive thyroid
- Having too much iodine in your diet or in medicines, such as amiodarone
- Having a noncancer tumor in the pituitary gland that makes your thyroid overactive
What are Causes of Thyroiditis?
Hashimoto's thyroiditis (chronic lymphocytic thyroiditis)
Hashimoto’s thyroiditis is a type of inflammation of the thyroid gland that results from an autoimmune process. It is the most common cause of Hashimoto’s hypothyroidism (in which the inflammation results in an underactive thyroid gland) in the U.S. However, some individuals with Hashimoto's thyroiditis may never develop hypothyroidism and thus never have any symptoms.
Infectious thyroiditis
Infectious thyroiditis is inflammation of the thyroid gland resulting from an infection in the thyroid. Patients with this will usually have neck pain, enlargement of the thyroid gland, and symptoms of an infection, such as fever and generalized body aches.
Painless thyroiditis
Painless thyroiditis is an inflammation of the thyroid gland in which there is a short period of both hyperthyroidism and hypothyroidism. The thyroid gland is not painful. Both usually resolve without treatment. Painess postpartum thyroiditis refers to this disorder when it occurs in women who were recently pregnant.
Drug-induced or radiation thyroiditis
Inflammation of the thyroid gland may also occur in individuals who are taking certain medications, including amiodarone, lithium, and interferon. Radiation of the neck can also result in thyroiditis. The hyperthyroid and hypothyroid phases of thyroid inflammation can be managed usually with medications alone.
Fibrous thyroiditis (Riedel's thyroiditis)
Fibrous thyroiditis is an extremely rare condition in which the thyroid becomes hardened from a significant inflammatory process in the thyroid that extends locally in the neck. Surgery may be required to treat this condition.
Prepare For Your Visit
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Hyperthyroidism Videos
Surgery for Graves' Disease: Surgery for Graves' disease involves removing half or the entire thyroid (thyroidectomy).
Update in Graves' Disease: UCLA endocrine surgeons Dr. James Wu and Dr. Masha Livhits review current treatments of Graves' disease.
Diagram of Patient-Reported Outcomes
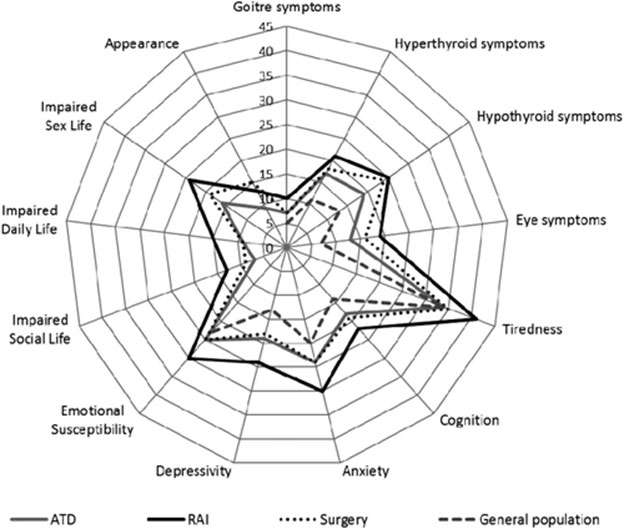
FIG. 1. Mean Thyroid-Related Patient-Reported Outcome (ThyPRO) questionnaire scale scores, adjusted for sex and age among patients with Graves' disease, treated with antithyroid drugs (ATD), radioactive iodine (RAI), or surgery, as well as scores from a general population sample. Patients in the RAI group may have received ATD but not surgery. Patients were allocated to the surgery group if they had received thyroid surgery, irrespective of previous ATD or RAI treatment. Items in four scales (impaired social life, impaired daily life, impaired sex life, and appearance) are asked with attribution to thyroid disease and cannot be answered by respondents from the general population. Scale scores range from 0 to 100, with higher scores indicating worse health status. .
Meet Our Endocrine Specialists:
Westwood Endocrinology
Westwood Pediatric Endocrinology
Torrance (South Bay Endocrinology)

Staff


Encino Endocrinology
Westlake Village Endocrinology
Find your care
We deliver effective, minimally invasive treatments in a caring environment.
Call 310-267-7838 to connect with an expert in endocrine surgery.











