Radiation Therapy
Find your care
Our radiologists lead the way in prostate imaging. We offer the newest techniques to better detect and stage prostate cancer. Call 310-481-7545 to find out more about prostate imaging and treatment options.
History
- 69 year-old, BPH gradual
- PSA rise 1.6 → 4.8 ng/dl
- Abnormal digital rectal exam → Biopsy: Gleason 5+4=9
Imaging
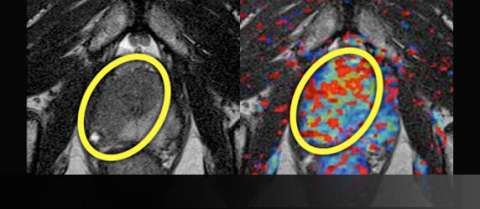
LEFT: T2-weighted image prior to treatment shows large, low-signal mass (yellow oval) on the right crossing midline anteriorly
RIGHT: Color perfusion map shows correspondingly increased perfusion (yellow-green pixels) with washout (red pixels)
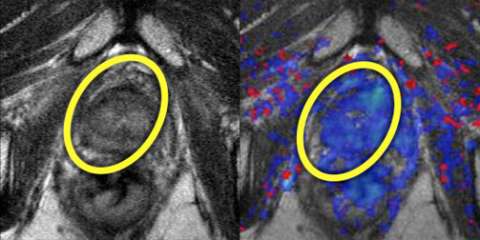
LEFT: T2-weighted image after treatment shows normalization of T2 signal with reappearance of the normal peripheral-transitional zone border.
RIGHT: Color perfusion map shows correspondingly decreased perfusion (blue pixels) consistent with response to treatment.
Example Report (Prior to Therapy) test
* Findings
No suspicious lymph nodes or bone lesions
Prostate measures 58 gm with mild prostatic hyperplasia
A single suspicious area is identified:
| Location | Bilateral anterior & right posterior |
| Size | 2.8 cm |
| Capsule | Involvement posterolaterally |
| T2 | Asymmetric, ill-defined |
| Perfusion | Abnormal |
| Overall suspicion | High (4/5) |
Seminal vesicles and neurovascular bundles appear normal
* Impression
- Technical quality: excellent
- Large right lesion crosses midline anteriorly and extends to capsule
- Organ-confined disease - no suspicious lymph nodes or bone lesions
Advantage: UCLA Prostate MRI
- Although PSA remains the mainstay of treatment monitoring, MRI can add value when there is concern for residual disease
- Removable table (GE HDxt or Siemens Skyra) allows for imaging after external patient mold is applied for registration with radiation planning.