UCLA Rheumatology Musculoskeletal Ultrasound
Find your care
Our rheumatologists are experts in all types of autoimmune diseases and joint conditions. To learn more, call 310-825-2631.
Musculoskeletal Ultrasound has become a popular method of non-invasive imaging technique in the field of rheumatology. Rheumatologists receive specialized training in musculoskeletal ultrasound to acquire the expertise for accurate utilization and interpretation of the ultrasound results. Due to the quick accessibility of information, it provides valuable diagnostic information and early detection for better management of our diseases.
Ultrasound allows visualization of joints, tendons, ligaments, muscles, and joint stability in real time, giving us a dynamic assessment of these structures. Due to the complexity of our diseases and the challenges we face with the diagnosis in early stages, this imaging modality plays a vital role in detecting inflammatory arthritis in the very early stages in a cost-effective manner.
The real-time imaging has not only enhanced the accuracy but also the precision of our ultrasound-guided procedures, making this a well-tolerated procedure in a convenient and flexible approach.
Musculoskeletal ultrasound has been evolving in the field of rheumatology and contributing to better outcomes for our patients as the research continues.
MSK Diagnostic Ultrasound
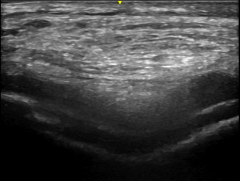
Musculoskeletal ultrasonography is a safe and painless imaging technique that uses soundwaves to evaluate bones, tendons, ligaments, nerves, and the joint as a whole. It does not use radiation and can be done even in pregnant women. This is a specialized exam performed in “real time” by a physician trained in MSK ultrasound.
An ultrasound gel is applied on the skin and the joint is scanned by moving the ultrasound probe to look for evidence of disease or inflammation. During the exam, you may be asked to move the joint so we can better evaluate the muscle, tendon, or ligament involved. Your doctor will be able to see the images of your joint through the screen and can discuss the findings with you as they see them.
Using MSK ultrasound, we can diagnose a range of musculoskeletal conditions including tendonitis, bursitis, carpal tunnel syndrome, gout, pseudogout, and inflammatory changes seen in rheumatoid arthritis or psoriatic arthritis.
Ultrasound Guided Procedure
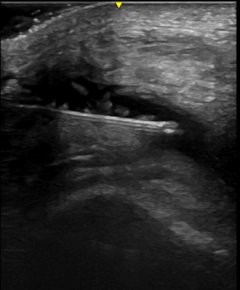
Injections have historically been performed using touch to identify physical landmarks, without the ability to confirm the accuracy of the injection. Ultrasound can be used to help providers improve the accuracy and effectiveness of injections.
During an ultrasound-guided injection, the needle can be visualized in “real time,” and adjustments can be made if needed. Ultrasound guided injections have been shown to reduce injury, have less side effects, and improve patient comfort. Both steroids and hyaluronic acid injections can be done under ultrasound guidance.
Salivary Gland Ultrasound
Sjogren’s disease is a chronic systemic autoimmune disorder that primarily affects the exocrine glands and usually presents as dry eyes and dry mouth. Salivary gland ultrasound is a non-invasive imaging technique that plays a crucial role in diagnosing the disease. In this procedure, high-frequency sound waves are used to create detailed images of the salivary glands, helping rheumatological patients and their doctors to assess the extent of glandular involvement. By visualizing abnormalities such as glandular enlargement and inflammation, ultrasound can help in detection and differentiation from other conditions with similar symptoms. With its safety, accessibility, and ability to provide valuable insights into disease activity, salivary gland ultrasound emerges as an indispensable tool in the management of Sjogren's disease.
Synovial Biopsy
We are able to offer ultrasound guided synovial biopsy for diagnostic and research studies. US guided synovial biopsy is similar to an US guided joint injection or aspiration. The skin over the joint is cleaned with antibacterial scrubs. The skin and joint capsule is numbed with lidocaine. Ultrasound is used to guide the needle directly to the joint capsule. Fluid and/or synovial tissue can then be removed through the needle. The synovial biopsy needle is introduced with a guide. The needle and guide are slightly larger than the joint injection/aspiration needle. The guide is left in place while the biopsies are done. Four to ten biopsies can be done through the guide. Once the guide is in place, the needle does not go through the skin again.
Synovial biopsies are done in our US procedure room under strict sterile procedures, (gowns, gloves, and sterile fields.)
Joint injections or aspirations can be done in our US procedure room or in our doctors’ offices, (also under sterile procedures but gowns not needed.)
Education
Education of the next generation of rheumatologists in ultrasound is of paramount importance, with understanding that musculoskeletal ultrasound has a high impact on the diagnostic, prognostic, and therapeutic clinical utility. In 2015, the first Rheumatology Fellowship Musculoskeletal Ultrasound Training Program was developed to provide a robust ultrasound training program for UCLA rheumatology fellows.
The comprehensive curriculum provides didactics and hands-on training through 11 two-hour workshops: knobology, hand, wrist, elbow, shoulder, feet, ankle, knee, hip, pathology, and injection. Additional education is provided on rheumatology subspecialty areas of the use of ultrasound in rheumatology: salivary glands, vasculitis, skin, muscle, and synovial biopsy.
Rheumatology fellows are encouraged to take advantage of clinical blocks taught by our eight RhMSUS certified faculty to further enrich their educational experience. In addition, rheumatology fellows have the opportunity to involve themselves in ongoing research projects in musculoskeletal ultrasound within the division.














