Esophageal Stricture
Find Your Care
We work as a team to provide outstanding esophageal care. Call 833-373-7674 to connect with a specialist at the UCLA Robert G. Kardashian Center for Esophageal Health.
What is an esophageal stricture?
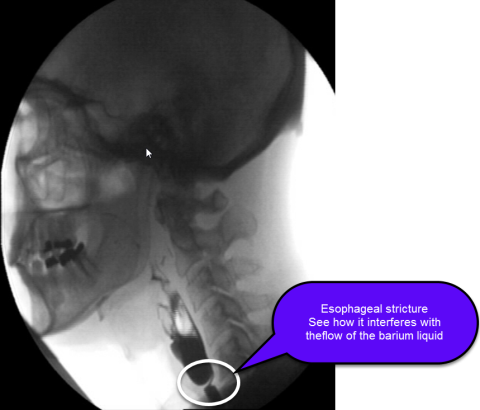
The esophagus is a muscular tube that connects the mouth to the stomach and is the conduit for food bolus to pass from the throat to the stomach. An esophageal stricture is a narrowing of the esophagus (see figure).
What causes an esophageal stricture?
Generally, anything that injures the esophagus can cause scarring, which ultimately can lead to a symptomatic narrowing of the esophagus. The most common cause of an esophageal stricture is long-standing gastroesophageal reflux disease (GERD), where stomach acid backs up from the stomach into the esophagus and causes esophageal inflammation, which can lead to scarring and narrowing over time. Less common causes of an esophageal stricture include eosinophilic esophagitis, radiation therapy, treatment for esophageal varices (banding or sclerotherapy), caustic ingestions, esophageal surgeries, cancer, and rare dermatologic diseases that involve the esophagus. Congenital esophageal strictures and webs also exist. An esophageal stricture rarely may also result from external compression of the esophagus.
What are the symptoms of an esophageal stricture?
The main symptom of an esophageal stricture is dysphagia, meaning difficulty in swallowing. This may manifest as a sensation of food sticking or feeling of delay in food passage in the throat, chest or upper abdomen. Not all strictures cause symptoms, but symptom presence and severity usually correlate with the degree of esophageal narrowing. At first, there may be difficulty with swallowing solid food or pills, but as the narrowing worsens, there may be difficulty with swallowing liquids as well. Patients may also experience heartburn, regurgitation, pain with swallowing, or unintentional weight loss.
How is an esophageal stricture diagnosed?
Specific testing is necessary to diagnose an esophageal stricture. An esophageal stricture can be diagnosed on a barium swallow study and/or upper endoscopy (EGD). In general, an upper endoscopy is needed to confirm the diagnosis and evaluate for the cause of the stricture.
What are the treatment options for an esophageal stricture?
Esophageal dilation is the initial treatment of choice for symptomatic benign esophageal strictures, in addition to the treatment of the underlying cause. Although there are different types of dilators, balloon dilators are typically used and this can often be performed at the time of endoscopy. Depending on the severity and complexity of the stricture, several sessions of dilations may be required to achieve adequate symptom relief and there may be a need for ongoing episodic dilation if symptoms recur. For complete strictures of the esophagus due to radiation therapy, anterograde-retrograde dilations are necessary. There is a rare risk of perforation with esophageal dilation. For some patients who do not achieve adequate symptom relief despite frequent dilations, other options may include corticosteroid injections into the esophageal stricture after dilation to reduce stricture recurrence or temporary placement of esophageal stents.