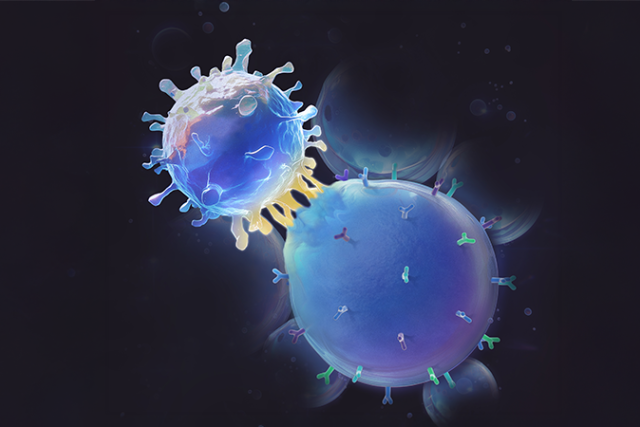
UCLA researchers have created a synthetic, cell-like material with viscous and elastic properties that better mimics immune system’s natural mechanism for activating T-cells. The discovery can help mobilize the type of white blood cell that plays a critical role in protecting the body form infection and helping fight cancer and other diseases.
To kickstart resting T-cells into a search-and-destroy-pathogens mode, the immune system relies on antigen-presenting cells that inform T-cells about the presence of an intruder and signal them to take action in defending the body and eliminating the threat. How to make the cell-mediated immune response kick in faster and more effectively is the focus of a UCLA-led study recently published in Nature Biomedical Engineering.
The team introduced its new synthetic viscoelastic antigen-presenting cells, or SynVACs, which more closely mimic the natural viscoelastic, or springy, property of antigen-presenting cells. This approach is different from previous efforts in making artificial antigen-presenting cells that have solely focused on rigid materials or magnetic beads widely used in scientific research as cell substitutes.
“Understanding the complex mechanisms through which T-cells recognize antigens and kill tumor cells remains one of the core challenges in immune engineering,” said study co-principal investigator Song Li, Chancellor’s professor of bioengineering at the UCLA Samueli School of Engineering. “Our research demonstrated that viscoelasticity, not just the stiffness of materials or cells, plays a crucial role in modulating T-cell activation, expansion and further development into specialized T-cells.”
In the team’s experiments, SynVACs outperformed traditional methods by promoting better T-cell expansion and function. This included increasing the population of cytotoxic T-cells — cells that actively find and neutralize intruder cells, such as cancer cells — and generating more memory T-cells, stem cell-like cells that are important for long-term immunity and cancer therapies.
“This breakthrough has the potential to improve cancer therapies, especially for patients with solid tumors, by enhancing the body’s ability to target and destroy cancer cells more effectively, while also reducing the risk of the cancer coming back,” said co-principal investigator Lili Yang, a UCLA professor of microbiology, immunology & molecular genetics.
SynVACs are made of alginate, a biocompatible material, and engineered to simulate both the stiffness and viscoelastic properties of natural cells. A microfluidic system is used to precisely control the size, shape and mechanical properties of these synthetic cells. Their viscoelasticity allows the synthetic cells to better replicate the organic cell interactions detected by T-cells, leading to significantly improved T-cell activation, expansion and functionality.
Experiments were conducted on humanized mouse models and resulted in increased activation of memory T-cells. Chimeric antigen receptor T-cells produced by SynVACs eliminated or suppressed tumor growth in both lymphoma and ovarian cancer.
The paper’s three co-first authors are UCLA Samueli bioengineering research scientist Leo Zeyang Liu; postdoctoral scholar Charlie Yan-Ruide Li of microbiology, immunology & molecular genetics; and recent bioengineering Ph.D. graduate Raymond Youcheng Yang.
Li and Lili Yang are also faculty members with the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA and the UCLA Jonsson Comprehensive Cancer Center in the David Geffen School of Medicine at UCLA. Lili Yang is also a member of UCLA’s Molecular Biology Institute and the Parker Institute for Cancer Immunotherapy.
Other study authors are affiliated with the UCLA departments of Bioengineering; Microbiology, Immunology & Molecular Genetics; Chemistry and Biochemistry; and the UCLA School of Dentistry.
The research was supported by a UCLA Jonsson Comprehensive Cancer Center seed grant, a UCLA Broad Stem Cell Research Center Innovation Award, a grant from the National Institutes of Health, a Discovery Stage Award from the California Institute for Regenerative Medicine and an Ablon Scholars Award.
The UCLA Technology Development Group has filed for a patent on the technology and provided innovation funds to facilitate its further development as a medical device, which is currently in the preclinical stage. The team is working to move the research through regulatory approval processes before entering clinical trials.