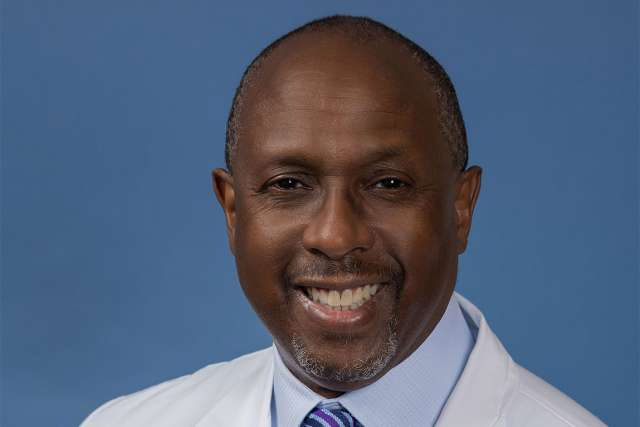
Vincent Rowe, MD, division chief of Vascular and Endovascular Surgery at UCLA Health, knows the devastation peripheral artery disease can unleash on patients.
“When it gets to a more severe state, it will impact their ability to heal a small opening or even lead to the tissue in the area dying,” Dr. Rowe said. “It is one of the biggest causes of amputation.”
The most significant challenge is “getting to the patient early enough because we don’t screen for PAD,” Dr. Rowe said. The needle hasn’t moved despite legislation in Congress to require greater insurance coverage of screening, which has stalled, and in spite of having maps that precisely show the areas where amputation rates due to PAD are higher, he said.
Where Dr. Rowe has been able to make a difference is in using a multidisciplinary approach to treatment. He gives the example of a gardener in his 60s who was told he needed an above-knee amputation by a practitioner about two hours away. The patient had a severe infection in his bone and tissue loss at the heel.
“He basically had the podiatrists take care of the infections in the bone and the heel,” Dr. Rowe explained. “The plastic surgeons then covered the defect in the heel with tissue transfer from the groin to the foot. Later in his course, I did a boutique procedure to get blood flowing to the foot. He only ended up losing a part of his toes instead of his leg above the knee. And with the help of our wound care specialist, all of his incisions and open wounds healed. The patient was ambulatory after six to eight months of treatment.”
Potential of multidisciplinary care
This man is an example of someone who greatly benefitted from a multidisciplinary approach. Such an approach also enables medical teams to take on more difficult cases, said Dr. Rowe. Here, he sees significant potential.
“We already have a wound care center with a staff of nurses and doctors who are interested in this area,” he said. “We have a hyperbaric chamber to put patients who have significant infection, which gives them a better chance of healing.”
UCLA Health has a cohort of podiatrists and a procedural unit where “we can perform some procedures such as minor debridement of the foot or angioplasty of the artery of the leg without the patient having to be admitted,” Dr. Rowe said. “We already have so much in place. It’s just a matter of us finally tying it all together, and we’re close to doing that.”
PAD cases bring an elevated level of complexity. At UCLA Health, a common scenario is seeing patients who have had endovascular stents placed by other community physicians, and the stents have, Dr. Rowe said.
“Recently, we had one patient who had extensive stents from the belly button to the knee and all had failed,” he said. “We had to figure out how to work around that and how to get blood flow to the patient’s leg without amputating the leg.”
In this case, Dr. Rowe’s team chose to bypass the failed stents. In other cases, he says, they could reopen the stent and remove the scar tissue inside it. UCLA Health has experts adept at both procedures, which positions them uniquely to tackle these challenges, he said.
Future of PAD treatment
UCLA Health also is on the cusp of further innovation in treating PAD. Dr. Rowe gave the example of Dr. John Rollo, a UCLA Health vascular surgeon, who successfully implanted the first bioabsorbable stent on the West Coast.
“This is a big technological change that will undoubtedly help improve patient outcomes,” he said. It is an exciting time, Dr. Rowe said, particularly because UCLA Health has a robust mix of all specialties to treat PAD, combined with the ability to reach the communities that need this care the most.
“It’s going to be a very comprehensive approach to treating PAD given the expertise we have in open surgery, endovascular surgery, wound care, plastic surgery, podiatry, hyperbarics and outreach,” he said.