The diseased tissue of early-stage lung cancers can appear like hard marbles within the soft, sponge-like lungs.
“Lung cancers often exist as solitary nodules or masses within the complex anatomic architecture of the lung,” says Bryan Burt, MD, chief of the division of thoracic surgery at UCLA Health and a professor of surgery in the David Geffen School of Medicine at UCLA.
When these nodules or masses are extracted, a certain amount of functioning lung tissue surrounding them is removed as well. This is called the surgical margin.
The margin must be assessed to ensure there is no microscopic spread of cancer cells. But the current testing method is onerous and time-consuming.
While the patient is still under anesthesia, the tissue at the cut line is rushed from the operating room and brought to a lab. There, a pathologist freezes and slices the tissue and examines it under a microscope.
If the margin is negative, the tumor has been resected. But if any cancer cells are present, more lung tissue must be removed, and the frozen section technique must be repeated until the margin is clear.
This can take anywhere from 30 minutes to an hour for results.
“This is a time-honored method of real-time evaluation of surgical tissue that has limitations that we are trying to improve upon,” says Dr. Burt.
So, he is leading research on new technology: a pen-like tool that can be directed on the patient’s lungs during surgery.
The new device not only eliminates the need to carry lung tissue out of the operating room into a lab. Its analysis of healthy and cancerous areas is done in seconds with high accuracy.
Dr. Burt is currently investigating its ability to evaluate the surgical margins, so no cancer cell is left behind in the patient.
“It would save an enormous amount of time in the operating room,” Dr. Burt says, “and that savings directly benefits the patient.”
The new technology plays an important part in treating lung cancer. The disease is the leading cause of deaths from cancer, more than those due to breast, colon and prostate cancers combined.
Lab testing
Before it can be used in surgery at UCLA Health, the pen tool is undergoing intensive testing and training in a research setting.
Lung tissues from surgeries are evaluated in an 11th floor laboratory in the UCLA Health Jonsson Comprehensive Cancer Center.
There, a small piece of tissue is analyzed with the MasSpec Pen, a device invented by Dr. Burt’s collaborator, Livia Eberlin, PhD, at Baylor College of Medicine. This project is supported by a R01 grant from the National Institutes of Health awarded to Dr. Burt and Dr. Eberlin.
In the Cancer Center lab, Alberto Antonicelli, MD, a research scientist in Dr. Burt’s group, fits a disposable probe – 3D-printed nearby with a resin that is biocompatible with human tissue – to the end of the pen. He holds it steady over the tissue on a slide.
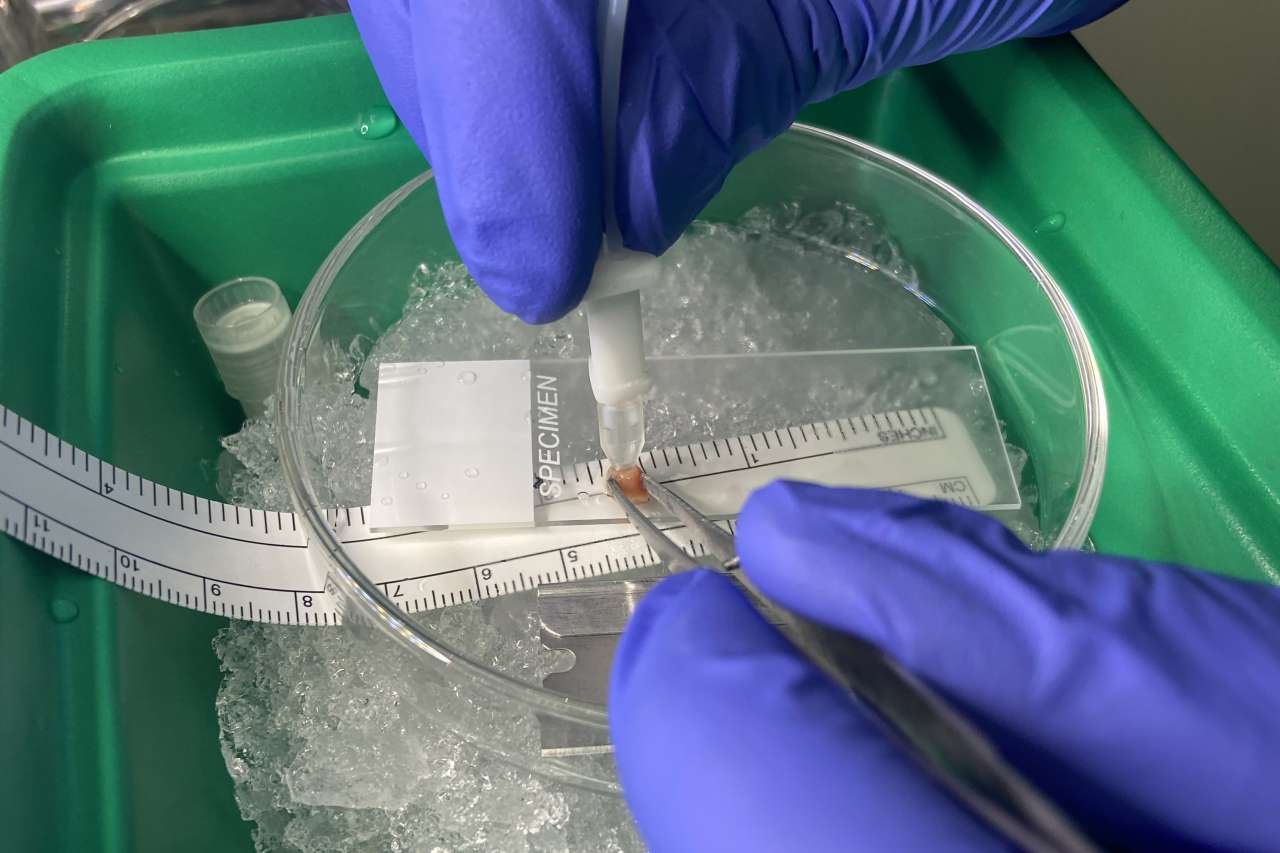
A single droplet of purified water emerges from a channel at the tip of the pen, suspended in the interface between the pen and the tissue.
A few seconds later, the pen’s vacuum system draws the water back up another channel and into a long tube connected to a mass spectrometer. The machine examines the droplet, now containing the tissue’s molecular profile.
“We can identify a tissue type in real-time with the MasSpec Pen,” says Dr. Antonicelli. “It’s like finding a criminal, by analyzing their fingerprint and identifying who that person is.”
Certainly, the criminal to be detected is cancerous tissue. But the machine also analyzes healthy parts of the lung. The cumulative data trains the technology’s algorithm to determine the differences between the two.
The rigorous testing of hundreds of samples from UCLA Health, Baylor College of Medicine and a biorepository maintained by the National Cancer Institute will help refine the pen tool's algorithm ahead of its debut in real-time surgery.
And when that happens, the equipment now in the lab could be rolled directly into the operating room.
Hospital deployment
Clinical testing will be an opportunity to introduce the MasSpec Pen into a surgical setting and fine-tuning its precision.
Just as the tool now tests samples on a slide, in surgery it can directly analyze the lung tissue in the patient – and provide an evaluation of the surgical margin within seconds.
“I am very excited about the promise of this platform for improving the care of our patients,” Dr. Burt says. “I look forward to collaborating with our pathology team to advance this technology.”




