Radiofrequency ablation (RFA) may not be the first thing that comes to mind when considering cancer treatments. Surgery, chemotherapy, radiation, and most recently, immunotherapy, are the standard treatments for various types of cancer.
But Jay Acharya, MD, a diagnostic neuroradiologist at UCLA Health, says adding RFA to the repertoire of treatments can provide an effective option for the growing number of cancer patients who are living longer but are getting diagnosed with secondary or metastatic spinal cancer, which is cancer that starts in another part of the body and spreads to the spine.
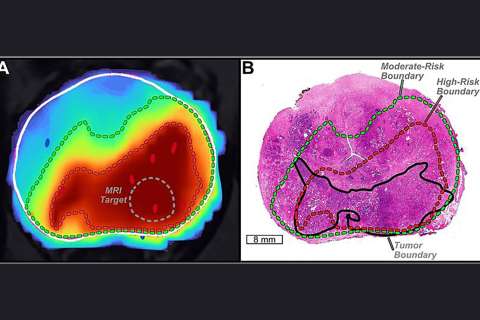
Part of Dr. Acharya’s job involves diagnosing where a tumor is located in the vertebra by reading magnetic resonance imaging (MRI) scans. This enables him to assess whether a patient is an appropriate candidate for RFA treatment. The minimally invasive procedure involves using a needle to gain access inside the bone and precisely inserting a probe to burn a tumor, a procedure known as thermal ablation. The heat is generated by radiofrequency waves.
In this interview, Dr. Acharya explains his work in radiology and why RFA is an effective supplementary cancer therapy.
Q: What inspired you to go into neuroradiology?
Dr. Acharya: I wasn’t that particularly interested in radiology in medical school, but I had a mandatory rotation in the specialty. When I started that rotation, I got a better understanding of what it is a radiologist does, the value that a radiologist plays in the entire health care system, and how patients are diagnosed and ultimately treated. While you don’t interact as much with patients, you work closely with other clinicians at a very high level and have deep, meaningful conversations about patients. This type of collaboration was fascinating.
During my residency, I was immediately drawn to neuroradiology as I found the patients to be complex, the anatomy very intricate, and the disease processes not very well understood. It was during this time where I found the value in doing neuroradiology procedures. I was still able to work with the other clinicians at a high level, but I was also able to interact with patients more and determine how I can help ease their pain or discomfort.
Q: What does a normal day look like for you?
Dr. Acharya: I perform minimally invasive procedures to treat and manage pain for patients with spine fractures, disc herniation, or a pinched nerve. I also treat patients who have a cerebrospinal fluid leak – when the protective fluid surrounding the brain and spinal cord seeps out of the tissue – by repairing the tear. But my main focus right now is spine oncology – it’s an area that I want to build and grow. Part of this work involves conducting a biopsy in the tissue of the spine to determine if a patient has a malignant or benign tumor.
Q: Can you talk more about your work in spinal intervention for oncology?
Dr. Acharya: Medicine has really advanced as a whole. There are a lot of new pharmaceutical, immunotherapies, and biologic treatments that have emerged that target different tumors. As a result, we're seeing cancer patients that are living longer, but are also getting secondary spinal cancer.
As a neuroradiologist who reads the spine MRIs in which we diagnose these findings, I have a strong, three-dimensional understanding of where the tumor is located. One of the aims of RFA is to position the needle and probe in the correct location. When a tumor is located inside the bone I use RFA, and when it’s located around the spine, I use cryoablation to freeze the tumor. They both effectively kill the tissue. Afterward, I insert cement to stabilize the bone because it’s susceptible to fracture.
RFA is part of a holistic treatment methodology. I work with radiation oncologists and spine surgeons to try to find the right patients to treat because every patient is a little bit different, and the tumor is a little bit different. I treat patients with RFA before or after they receive radiation, or patients who have had prior radiation and are not a candidate for additional radiation due to potential damage to the spinal cord, nerve roots, or other nearby structures.
Q: What is the future of radiofrequency ablation in treating cancer?
Dr. Acharya: I have treated patients who have no disease progression at the site on the spine and discuss RFA at national and international conferences, but I’d love to get to a point where I work with different specialties to get meaningful data that can be published to create more of an understanding and an awareness of how effective this can be. My ultimate, overarching goal would be for RFA to be considered as an option when clinicians think about how to treat spinal cancer.