Human papillomavirus (HPV) causes as many as 70% of oropharyngeal cancers, meaning cancers of the middle part of the throat, according to the U.S. Centers for Disease Control and Prevention. Many people don’t know the HPV vaccine can protect against this, according to Lauran Evans, MD, MPH, a PGY-5 otolaryngology resident in UCLA’s Department of Head and Neck Surgery.
“Around 2018, when new data was just coming out on this, I was in medical school,” Dr. Evans says. “I talked with my medical school colleagues, residents and professors about it. I found it shocking that no one knew HPV caused throat cancer, and that we could prevent it so easily if people would just become vaccinated.”
Understanding HPV
A person can get the HPV virus from skin-to-skin and sexual contact. Recent studies also suggest it could be spread by saliva.
“HPV causes a lot of different disease processes,” Dr. Evans says. “It can cause anything from hand/foot warts and genital warts, to warts in the airway, mouth and voice box.” HPV is also the most common cause of cancers of the oropharynx, genitals and cervix, Dr. Evans notes.
Though many healthy people can fight HPV off, some people can’t. That’s when it turns into warts and cancer. Vaccination is 99% effective against HPV-related disease, and is now recommended starting at age nine and can be given up to age 45.
“All genders and sexes should receive the HPV vaccine,” Dr. Evans says. Depending on when a person starts the vaccine, it’s given either in two or three doses.
Dr. Evans created an educational course about HPV and throat cancer during medical school. At first, it was for other students, trainees and doctors in areas including pediatrics, internal medicine, family medicine, obstetrics and gynecology, and head and neck surgery. Her goal was to equip them with the knowledge and skills to counsel their patients on HPV and offer vaccination.
According to Dr. Evans, after UCLA’s primary care residents attended the workshop, not only did their knowledge of HPV improve, but their patients’ HPV vaccination rates also went up.
“That’s been very powerful and rewarding,” she says.
Expanding impact
After giving the workshop for six years, Dr. Evans has recently been widening the audience to include more than providers.
“I have given three workshops to high school and college students so far,” she says. “We are also transforming it to be given at community centers, largely in the Black and Latinx communities through UCLA’s community outreach program.”
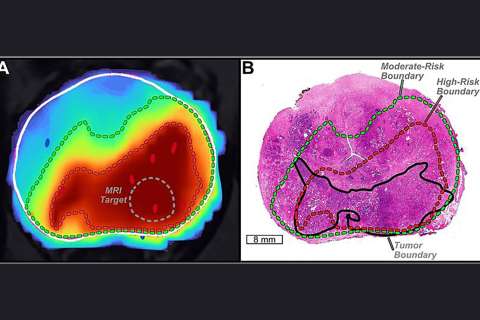
Dr. Evans is also contributing to several basic science projects to learn more about treating HPV-related throat cancer. One such project involves taking samples from patients with these cancers, imaging them with a fluorescence device and growing new tonsil tissue in a lab.
“We test new chemotherapeutic agents, medications and radiation dosages on lab-grown human tissue to develop therapeutic protocols for treating patients who have HPV-related throat cancer,” she notes.
Dr. Evans says that there’s a lot more to be done as far as teaching people about HPV and helping them get the vaccine.
“Right now, we aren’t doing well enough with HPV vaccination,” she says. “There is an epidemic of oropharyngeal cancer, meaning that every year the rates continue to rise. We could prevent all this illness and death if we could just increase HPV vaccination rates.”