Up to 40% of the U.S. population will experience hemorrhoidal disease in their lifetime, but many people are hesitant to follow through with care due to the pain and long recovery times associated with surgical treatment.
Internal hemorrhoids occur when hemorrhoid tissues inside the rectum swell, and sometimes bulge outside the anus, causing bleeding and discomfort. There are several risk factors, including age, prior pregnancy, diet, and bowel habits.
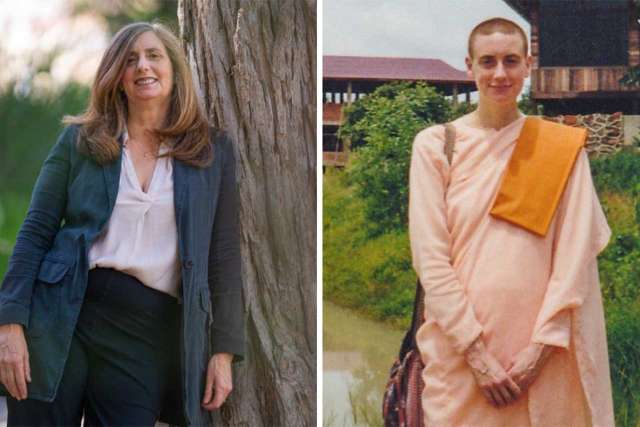
“Although surgery and trans-anal procedures can be very effective, some patients are concerned about associated pain and complications, and are looking for alternative options,” said Lucas Cusumano, MD, an interventional radiologist at UCLA Health and assistant professor of Interventional Radiology at the David Geffen School of Medicine at UCLA.
Now, however, a nonsurgical procedure performed by UCLA Health Interventional Radiology aims to make treatment more palatable. Interventional radiologists offer a minimally invasive procedure called hemorrhoidal artery embolization (HAE) designed to alleviate bleeding and gradually shrink the hemorrhoids.
During the approximately two-hour procedure, an interventional radiologist inserts a small catheter into the artery in the wrist or upper thigh using image guidance.
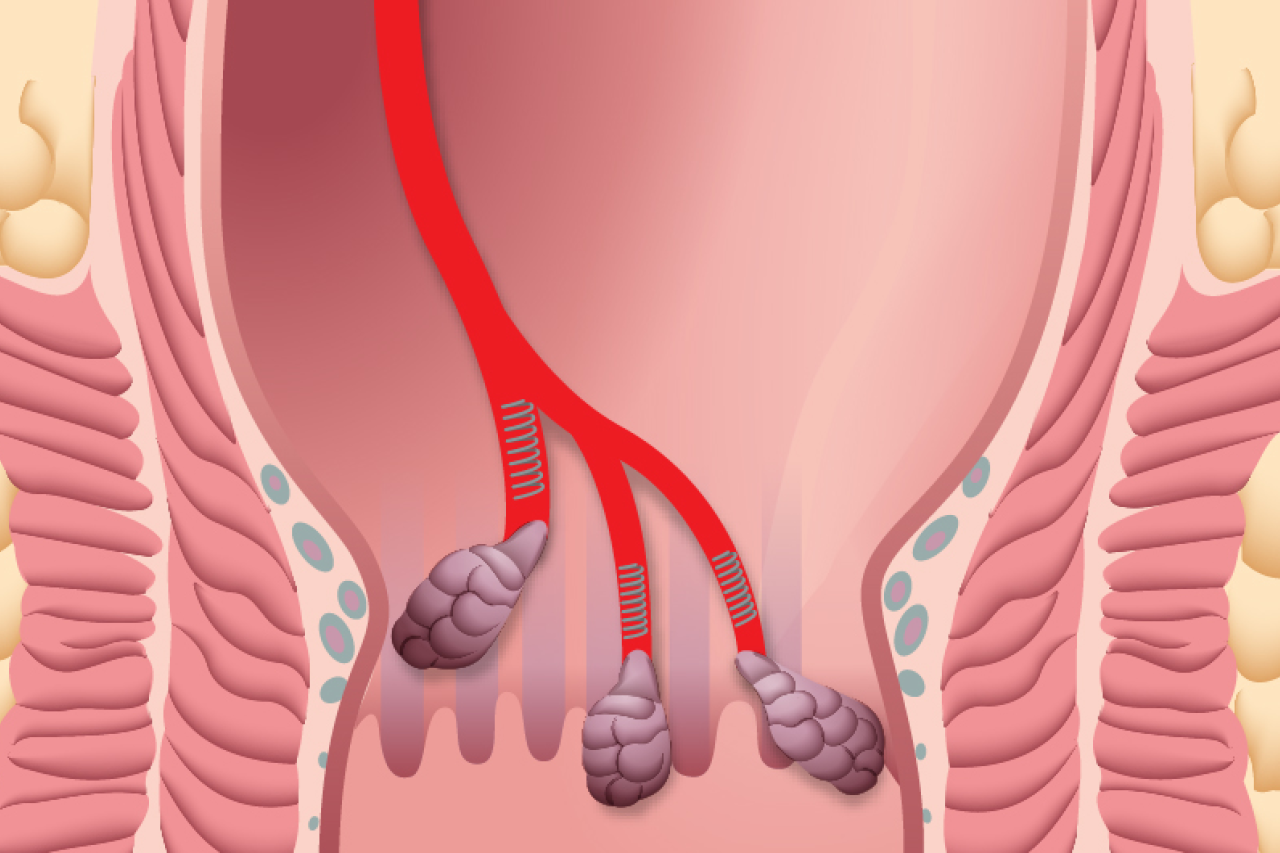
They then perform an angiogram, using contrast dye to identify the specific blood vessels supplying the hemorrhoids. Once located, a microcatheter is used to insert tiny particles and coils into the vessel to block off abnormal blood flow to the hemorrhoid tissue.
The procedure is performed in a single outpatient visit and patients are discharged the same day, with minimal recovery time.
Why consider HAE for hemorrhoids?
Many of the in-office treatments, such as rubber band ligation, doppler-guided hemorrhoidal artery ligation, and sclerotherapy, are only effective for early-stage disease and take multiple sessions, explained Jessica Stewart, MD, an interventional radiologist at UCLA Health and assistant professor of Interventional Radiology at the David Geffen School of Medicine at UCLA.
Symptoms can reoccur following these procedures, which can be uncomfortable, she added.
Surgery is often recommended for patients who have failed in-office treatments or have more advanced disease but is often followed by painful and prolonged recovery, Dr. Stewart added.
“A lot of patients don’t want to have a painful surgical recovery, can't take the time off work, or maybe aren’t ideal surgical candidates for any number of reasons, including being on blood thinners or having multiple other medical problems,” she said.
HAE doesn’t require hospital admission and can be performed with moderate sedation. Ideal candidates for HAE include patients with predominantly bleeding symptoms who failed, have contraindications to, or wish to avoid transanal procedures or surgery.
“Patients don’t have to have tried other treatments to undergo embolization, if they prefer it,” Dr. Stewart said, “and undergoing HAE also doesn’t prevent a patient from getting surgery in the future.”
Record of success
Widely performed in Europe, HAE has been found to be a safe and effective procedure to treat bleeding-related symptoms of hemorrhoids.
A recent randomized clinical trial of 33 patients found that HAE resulted in similar resolution of bleeding-related symptoms as hemorrhoidectomy, the commonly recommended surgical treatment. However, patients who underwent the surgery reported more adverse events, including swelling, wound openings, and anal fissures. None of these complications occurred in the patients who underwent HAE.
Since they began performing this procedure in 2022, Dr. Stewart and Dr. Cusumano have found high success rates across their patients.
One of Dr. Cusumano’s earliest patients was a new grandfather, who had previously tried rubber band ligation – which uses rubber bands to cut off blood supply to the hemorrhoids – to treat severe rectal bleeding.
“He said it was the most painful thing, and he flat-out refused to undergo rubber band ligation again,” Dr. Cusumano explained.
This experience led him to try HAE. “He went from a seven and a nine in one of our bleeding scales to a zero,” said Dr. Cusumano. After a month, his bleeding was completely resolved, and he was able to spend more time with his grandkids without worry.
What is the process for getting HAE?
Patients who contact the Interventional Radiology Clinic are first screened for existing internal hemorrhoids and what symptoms they are experiencing. Patients should have some documentation of internal bleeding hemorrhoids within the prior year, such as from an anoscopy (a scoped examination of the anus) or sigmoidoscopy (an examination of the lower part of the colon), to ensure they would be appropriate for treatment, said Dr. Stewart.
“We also make sure patients are up to date on their colonoscopies,” added Dr. Cusumano.
Once they are considered candidates for HAE, patients have a preliminary evaluation, in which care providers discuss symptoms and possible treatment options.
“We also talk about lifestyle modifications,” added Dr. Cusumano. “Regardless of the treatment, if your bowel habits aren't good, or if you’re not getting enough fiber, the recurrence rates are much higher,” he said.
Following the initial workup, patients are scheduled for a CT scan to visualize the anatomy of their blood vessels and identify the targets for embolization. They are then scheduled for the HAE, which is performed as an outpatient with “twilight” or moderate sedation, said Dr. Stewart.
Patients are discharged the same day, with follow-up scheduled for a month later to evaluate their response to the treatment, said Dr. Stewart.
“We’re here to help, and we’re happy to do a consultation, discuss it, and get them moved in the right direction, whether that is a treatment with HAE or not,” Dr. Cusumano said.