Research Day Program
Agenda
-
Time Location Event 8:00AM – 8:30AM Dr. Beatriz Solis Hall and Foyer Check-in, Breakfast, and Networking 8:30AM – 11:30AM Dr. Beatriz Solis Hall Formative Assessment and Competency-Based Evaluation Tools: Dr. Matt Yu 9:30AM – 10:00AM Break 10:00AM – 11:00AM Dr. Beatriz Solis Hall The Best of 2025' s Residency Leadership Summit (RLS): Drs. Dan Lee, Anita Wong and Denise Sur
-
Time Location Event 11:30AM – 12:00PM Dr. Beatriz Solis Hall and Foyer Research Day Check-in, Lunch, and Seating 12:00PM – 12:05PM Dr. Beatriz Solis Hall Welcoming Remarks and Keynote Speaker Introduction – by Gerardo Moreno, MD 12:05PM – 12:55PM Dr. Beatriz Solis Hall Keynote: “Aging in South Los Angeles: A Comprehensive Analysis of Health Challenges Among African American and Latino Older Adults in Service Planning Area 6 (SPA 6)” – by Dr. Mohsen Bazargan 12:55PM – 1:00PM Dr. Beatriz Solis Hall Keynote Q&A 1:00PM – 1:40PM Cabrillo, Catalina, and Mojave Poster Session 1
1:10PM and 1:25PM Abstract presenters will provide 60-second oral summaries of their projects in each breakout room
Throughout the 40 min Poster Session, we encourage attendees to visit all three break-out rooms to view all abstract and case report posters and ask questions of the authors.
1:40PM – 2:25PM Dr. Beatriz Solis Hall Lectern Session 1 (Moderated by Dr. Bruno Lewin) 2:25PM – 3:05PM Cabrillo, Catalina, and Mojave Poster Session 2
2:35PM and 2:50PM Abstract presenters will provide 60-second oral summaries of their projects in each breakout room
Throughout the 40 min Poster Session, we encourage attendees to visit all three break-out rooms to view all abstract and case report posters and ask questions of the authors.
3:05PM – 3:50PM Dr. Beatriz Solis Hall Lectern Session 2 (Moderated by Dr. Christopher Kuhlman) 3:50PM – 4:00PM Dr. Beatriz Solis Hall Closing Remarks (Dr. Parastou Farhadian) and Raffle Winners Announced
Venue Information & Navigation
-
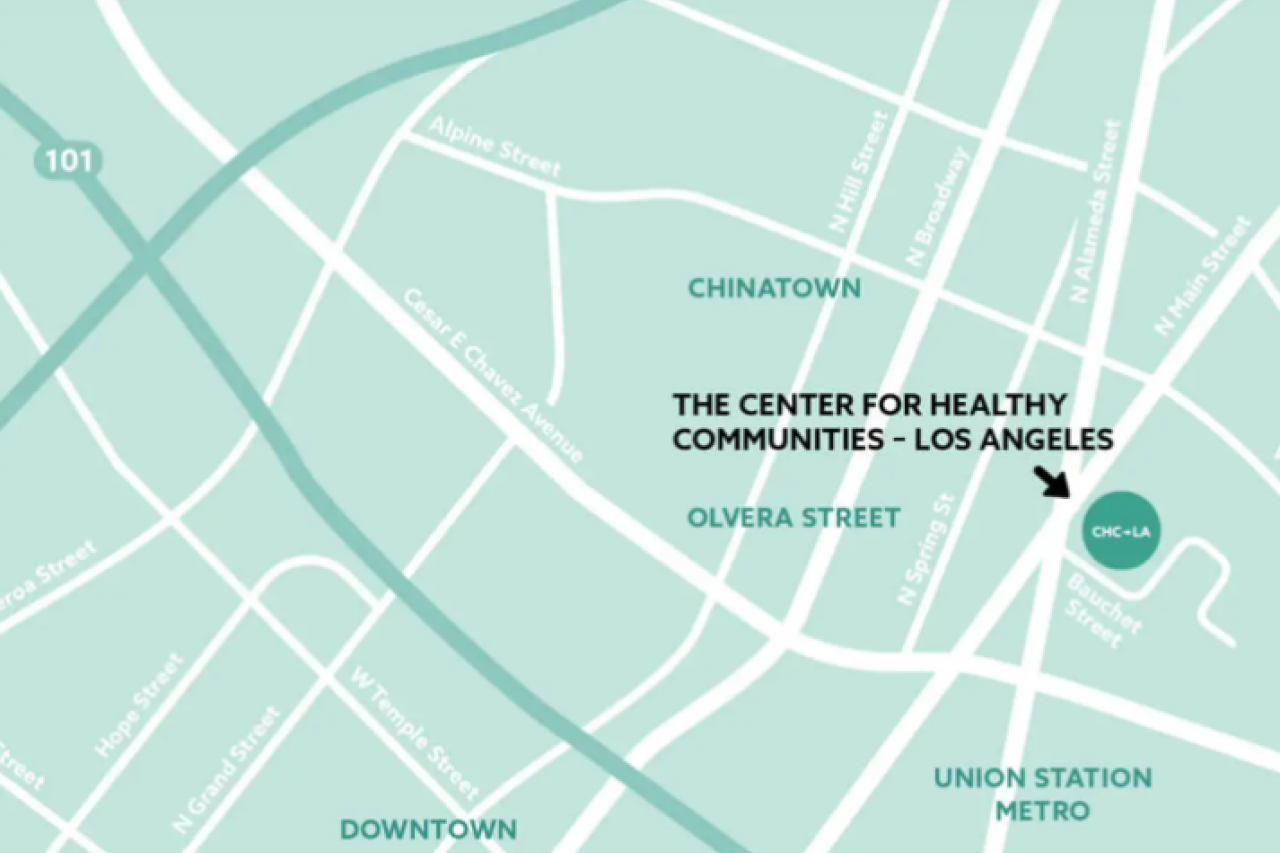
Research Day will be hosted at The California Endowment Center for Healthy Communities Los Angeles at . From Alameda St., turn onto Bauchet St. (stoplight) and continue to The California Endowment’s parking lot. We encourage attendees to carpool if possible. The venue is also easily accessible by public transportation, as it is within walking distance of the Union Station Metro. Free parking is available on a first-come, first-served basis. If the parking lot becomes full, we recommend you have cash as several nearby parking lots are cash-only.
-

Keynote (12:00 - 1:00PM)
-
Dr. Mohsen Bazargan, Ph.D. is a distinguished medical sociologist and gerontologist with more than four decades of experience in health services research. His work has maintained a sustained focus on aging, chronic disease, healthcare utilization, and the complex health challenges faced by underserved populations, particularly African American and Latino communities.
Dr. Bazargan has served as Professor and Vice Chair of Research in the Department of Family Medicine at Charles R. Drew University of Medicine and Science (CDU), where he has been a faculty member since 1993. He also holds an adjunct faculty appointment at the David Geffen School of Medicine at UCLA. His leadership roles at CDU include serving as President of the Academic Senate and as a member of the Board of Trustees—positions that underscore his longstanding dedication to academic governance and institutional advancement.
Throughout his career, Dr. Bazargan has authored more than 250 peer-reviewed publications and led numerous federally funded projects supported by the National Institutes of Health (NIH), the Health Resources and Services Administration (HRSA), and the Centers for Medicare & Medicaid Services (CMS). His research explores the structural, social, and behavioral factors that contribute to adverse health outcomes among medically underserved older adults. His findings have highlighted how chronic illness, financial strain, unmanaged pain, and limited access to care negatively impact health status and quality of life in these populations.
In response to the COVID-19 pandemic, Dr. Bazargan led the COVID-19 Health Ambassador Program (CHAP)—a faith-based, community health initiative that trained lay health advisors to educate and support African American older adults in resource-limited neighborhoods. He also conducted interventional research to reduce the risk of COVID-19 infection among residents of five public housing sites in South Los Angeles, further exemplifying his commitment to addressing urgent public health threats in structurally underserved communities.

Dr. Bazargan is deeply committed to mentoring and supporting junior faculty in engaging with communities and conducting research that improves health and quality of life among hard-to-reach populations. He currently serves as Principal Investigator on two federally funded research education and training grants, designed to enhance biomedical workforce capacity through academic enrichment, mentored research experiences, and structured career development in the areas of aging and population health.
His work continues to shape the national dialogue on healthcare quality, access, and system responsiveness, particularly regarding older adults facing complex and intersecting medical and social challenges. Dr. Bazargan’s lifelong research and leadership reflect a steadfast commitment to translating scientific evidence into practical, community-responsive strategies that improve individual and population health outcomes.
-
Dr. Mohsen Bazargan will be presenting on “Aging in South Los Angeles: A Comprehensive Analysis of Health Challenges Among African American and Latino Older Adults in Service Planning Area 6 (SPA 6)” from 12:00pm - 1:00pm in the Dr. Beatriz Solis Hall.
Poster Session 1 (1:00 – 1:40PM)
-
Predictors of Frequent Emergency Medicine Visits Among MediCAL Patients at UCLA
Authors: Ani Orujyan, Anais Panossian
Affiliations: UCLA David Geffen School of Medicine
Introduction: Emergency department (ED) overutilization is an ongoing challenge that has been estimated to cost $60 billion annually. Recurrent ED visits could be a reflection of gaps in primary care access, social determinants of health, and chronic disease management. A retrospective analysis of data from the National Hospital Ambulatory Medical Care Survey from 2005 to 2011 deemed 3.3% of all ED visits as avoidable, conservatively defined as discharged visits not requiring diagnostics, procedures or medications. Common complaints included toothache, back pain, headache, throat soreness, and mental health disorders such as depression and psychosis. Predictive modeling studies have demonstrated further that increased age, increase total number of chronic diseases, and general or digestive symptoms are strongly associated with non- avoidable ED visits, while younger age, injuries, and psychiatric symptoms are associated with avoidable visits. By analyzing different characteristics within the MediCAL population leading to avoidable ED visits, we can establish targeted interventions to improve healthcare delivery and decrease recurrent ED visits. There is currently limited institution-specific data at UCLA to help guide such interventions. This study aims to fill that gap by identifying social, demographic, and clinical predictors of ED overutilization among patients with MediCAL insurance assigned to UCLA primary care clinics. In doing so, we intend to implement targeted, systems-level interventions within UCLA primary care and ED settings to reduce potentially avoidable ED visits. Ultimately, when devising interventions, it is important to not penalize patients or restrict access to care, but rather consider provider-driven interventions such as patient education, discharge planning, and improving access to lower-cost options (urgent cares and telehealth).
Methods: This is a cross-sectional, quantitative study analyzing data from 1,558 MediCAL-insured patients assigned to UCLA primary care clinics. Patient-level variables include demographic factors (age, gender, housing status), primary diagnoses associated with ED visits, and healthcare utilization patterns. The dataset includes the number and type of ED visits, with categorization into avoidable vs. unavoidable ED encounters based on established clinical criteria.
Results: Pending data analysis.
Conclusion: Preliminary findings show that demographic and social determinants—including age, gender, and housing status — may be positively associated with increased frequency of emergency room visits. We anticipate further identifying additional predictors as data analysis progresses. Future directions include contacting a subset of patients to better understand the underlying causes of ED use not captured by electronic health data—such as barriers to primary care, unmet social needs, and perceived urgency of symptoms. These qualitative insights will guide the development of targeted interventions with a goal of reducing avoidable ED visits and improving continuity of care for MediCAL patients at UCLA.
Navigating Diabetes Treatment Options as a Spanish-Speaking Latino
Authors: Leslie Nuñez (1), Alejandra RivasDeras (1), Ann Marie Hernandez, MD (2)
Gerardo Moreno, MD (2)
Affiliations: (1) UCLA David Geffen School of Medicine; (2) UCLA Department of Family Medicine
Introduction: In 2021, over 38 million people in the United States had diabetes mellitus, accounting for 1 in 4 US healthcare dollars spent. Racial and ethnic minorities as well as those with limited English proficiency suffer from disparities in diabetes prevalence and control. Despite existing evidence supporting the use of sodium-glucose co-transporter 2 inhibitors (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP-1RA), studies have demonstrated racial, ethnic, gender, and socioeconomic disparities in their use. This study explores the experiences of Spanish-speaking, Latinx patients as they navigate decisions around diabetes treatment options.
Methods: We are conducting a qualitative study to explore how Spanish-speaking patients with diabetes make decisions about pharmacologic diabetes treatment options. Our study will include up to 30 semi-structured interviews. Inclusion criteria include self-identified Latino/an adults over the age of 18 with a diagnosis of insulin dependent diabetes. Participants will be recruited from two community partner sites, UCLA Family Health Center and Los Angeles County Mid-Valley Comprehensive Healthcare Center. Participants will have had at least two visits with a primary care provider in the last 12 months. Interviews will be conducted in person or virtually. Thematic analysis will be used to identify barriers and facilitators to decision-making. Descriptive statistics will be calculated.
Results: Using the six cognitive constructs of the health belief model, we developed a question guide consisting of four domains: knowledge of medications, body image, influence and cost. We postulate that emerging themes from the interviews will include language concordance, social network, affordability, self-esteem, use of social media, trust or lack thereof in the healthcare system and belief in oneself. We predict language discordance will be a major barrier to shared decision making, leading to decreased utilization of the medications of interest. High cost of medications, use of social media, and patient’s social network will be external cues to action while self-esteem and belief in oneself will be internal cues to action.
Conclusion: Results from this research study have clinical implications and will contribute to the literature examining disparities in GLP-1 RA and SGLT2i use and access. They will also inform future comparative studies with educational interventions tailored to weight loss and/or glucose control outcomes within the cultural context and shared decision-making processes in primary care. Lastly, they will guide the development of a survey and/or claims-based study of medication use among Latinos with diabetes in California.
Can Keloid and Hypertrophic Scars be Managed in a Primary Care Setting?
Authors: (1) Kushagra Tewari, (2) Lucas Karamanoukian, (2) Levon Karamanoukian, (3) Manuel Mendoza, MD
Affiliations: (1) Medical Student at the David Geffen School of Medicine, UCLA, (2) Brentwood High School, (3) Department of Family Medicine, UCLA Health Toluca Lake
Introduction: Keloid and hypertrophic scars represent abnormal wound healing processes that require early diagnosis and long-term treatment. Although the treatment of keloid and hypertrophic scars have traditionally been performed by subspecialists (dermatology and plastic surgery); primary care physicians also have the necessary skill set to treat the majority of keloid and hypertrophic scars in an outpatient clinical setting.
Methods: A retrospective cohort chart review was performed of one-hundred consecutive patients undergoing treatment for keloid and/or hypertrophic scars in a single-physician plastic surgery practice. Among the study participants, we reviewed demographics (Age, Gender); the prevalence of relevant skin co-morbidities (acne, eczema); surgical treatment types (outpatient surgery under local anesthesia or general anesthesia), medical treatment types (Pulsed Dye Laser, Fractional laser, Scar Massage), and pharmacologic treatment types (Intralesional Corticosteroid injection, Topical Tyrosinase Inhibitors) over a two year period (Jan 1, 2023 to January 1, 2025).
Results: 100 patients were identified (Avg Age: 38.6, 69% F). Majority of patients demonstrated evidence of Post-Inflammatory Hyperpigmentation (PIH, 75%) or Post-Inflammatory Erythema (PIE, 76%) on their scars. Prevalence of Acne (13%) or Eczema (2%) was low. Over a 2-year period, patients had a total of 1,041 treatments for keloid or hypertrophic scars. Treatments undergone included intralesional injections (94%), pulsed dye laser laser treatment (63%), CO2 Fractional Laser (17%), or topical preparations including polysiloxane or a tyrosine inhibitor (100%). 34 patients developed keloid or hypertrophic scarring from a previous surgery. 14 patients had surgical excision of keloid scars as a primary treatment modality (13 had surgery under local anesthesia, 1 had surgery under general anesthesia).
Conclusion: Our data demonstrates that the majority of treatments for keloid and hypertrophic scars in an outpatient specialty center are non-surgical; and involve combination medical therapy with intralesional injections, topical treatments, and laser scar therapy. Given a well-balanced medical and surgical knowledge base based on ACGME core-competencies in Family Medicine, primary care physicians have the requisite skill-base to diagnose, treat, and manage the majority of keloid and hypertrophic scar patients in an outpatient clinic setting.
Community-Based Approach to Assessing Healthcare Provider Awareness on the Environmental Impact of Inhalers in a Federally Qualified Health Center in Los Angeles
Authors: Vanessa De Haro (1), Monica Soto Noveron (1), Leslie Nuñez (1), Ky’Tavia Stafford-Carreker (1), Sherril Brown, MD (2), Gerardo Moreno, MD (3)
Affiliations: (1) UCLA David Geffen School of Medicine; (2) AltaMed Health Services Corporation (3) Department of Family Medicine at UCLA
Introduction: In the U.S., 25 million individuals have asthma, and marginalized, low-income communities near freeways, airports, and industrial zones are disproportionately impacted. Clinicians treat the health consequences of air pollution; however, the healthcare sector contributes to these pollution problems. The pressurized metered-dose inhaler (pMDI) is the dominant method of treating respiratory diseases such as asthma; however, its propellant is a known contributor to global warming. We will explore healthcare providers' knowledge of two types of inhalers with similar clinical efficacy and their differences in global warming effects.
Methods: A pre- and post- test survey will be administered to healthcare providers and clinical staff at Los Angeles County’s largest Federally Qualified Healthcare Center (FQHC), AltaMed, during April Grand Rounds. The survey will consist of nine questions assessing current prescription practices and awareness of environmental impact and clinical efficacy of two types of inhalers: pMDIs and dry powder inhalers (DPIs). A ten minute educational presentation will be delivered prior to administering a post-test with adapted questions. Descriptive statistics and paired t-tests will be used for a comparative analysis.
Results: We expect the educational intervention to improve healthcare providers’ understanding and influence their prescribing habits toward more environmentally friendly choices. We anticipate that baseline knowledge scores will be low, which will be followed by an apparent increase in knowledge scores on post-tests, showing a stronger awareness of inhaler-related environmental concerns. This intervention may show that even brief, targeted education can improve provider awareness and encourage more sustainable prescribing. It would highlight an opportunity to integrate environmental considerations into routine asthma care without compromising patient outcomes.
Conclusion: There is an urgent call for the healthcare field to reduce its carbon footprint. We anticipate this study will show that healthcare providers are unaware of the environmental impact of medications like pMDIs on global warming and highlight the need to increase environmental health literacy. It also highlights an opportunity to change the existing pharmacy formulary, first within entities like AltaMed, then followed by government programs like Medicaid and Medicare, to inform prescription practices and significantly reduce the carbon footprint.
Bridging Language Barriers in Dermatology: Assessing Spanish Proficiency and Training Gaps in California Dermatology Residents
Authors: Gladys Bello BS (1), Aldana Garcia MD (2) and Caroline N. Opene MD (2)
Affiliations: (1) Department of Family Medicine, DGSOM (2) Department of Dermatology, DGSOM
Introduction: California, home to over 15.8 million Hispanic individuals, faces disparities in dermatologic care from language discordance, causing delayed diagnoses and worse outcomes in melanoma and hidradenitis suppurativa (Ngo-Metzger et al., 2007). Despite benefits of language-concordant care, dermatology is among the least diverse specialties, with 4% of U.S. dermatologists identifying as Hispanic/Latinx (Pritchett et al., 2018). Few programs offer Spanish training (Ortega et al., 2020). This study assesses Spanish proficiency and training needs of California dermatology residents to inform the development of a dermatology-specific Spanish curriculum.
Methods: A cross-sectional, anonymous Qualtrics survey was distributed to dermatology residents (PGY2–PGY4) across 11 ACGME-accredited programs in California. The survey collected demographic data, self-assessed Spanish proficiency, frequency of Spanish-speaking patient encounters, and perceived gaps in training. Respondents assessed their comfort managing dermatologic conditions in Spanish and rated the adequacy of current language resources. Additional questions evaluated interest in specialized Spanish training and perceptions of how language concordance impacts diagnostic accuracy, treatment adherence, and patient trust. Descriptive statistics quantified proficiency levels and training gaps, guiding the development of standardized patient cases and a dermatology-specific Spanish curriculum.
Results: Of the 12 residents surveyed, 67% identified as female, with an even distribution across training years and half in PGY4. Spanish proficiency varied, with 17% reporting native fluency, 17% advanced, and 33% intermediate or below. Only 17% had received formal medical Spanish instruction in medical school, and none during residency. Confidence in medical Spanish use was variable, with only 33% feeling very confident. Notably, 67% of respondents reported Spanish-speaking patients comprising 26–50% of their clinical encounters, yet 83% indicated their programs offered no formal Spanish curriculum or resources. Importantly, 67% expressed interest in external training opportunities to improve proficiency. This is preliminary data, with data collection continuing through May 2025.
Conclusion: Our findings reveal that while many California dermatology residents regularly care for Spanish-speaking patients, only one-third feel very confident in their Spanish skills. The majority of residents express a clear desire for specialized training, underscoring a gap in residency education. These findings support the need for a dermatology-specific medical Spanish curriculum to address proficiency gaps and better prepare residents for language-concordant care, ultimately enhancing diagnostic accuracy, patient trust, and treatment adherence for Spanish-speaking populations.
Toxicity Profiles in Glioblastoma: A Patient-Centered Analysis of Adjuvant Therapy Tolerance
Authors: Amani Carson, BA (1), Travis Perryman, BS (1), Stuart Harper, BS (1), Amara Oniyah, BS (1), Lindsey Dudley, BS (2), Eliana Oduro (1), Alondra Delgadillo (1), Matt Kyle Bermudez (1), Kunal S. Patel, MD, (1, 3)
Affiliations: (1) Department of Neurosurgery, David Geffen School of Medicine, University of California Los Angeles; (2) The Intellectual and Developmental Disabilities Research Center and Department of Psychiatry and Biobehavioral Sciences, David Geffen School of Medicine, University of California Los Angeles; (3) Jonsson Comprehensive Cancer Center, University of California Los Angeles
Introduction: Delayed or discontinued adjuvant therapy is associated with poor neuro-oncological outcomes. This is particularly salient for patients with glioblastoma (GBM), which is both the most common and most aggressive primary brain tumor. Other oncological studies have shown that racial/ethnic minority, female, and older patients experience more disruptions in their chemotherapy and or radiotherapy courses due to disparities in adverse effects (AEs), but this is understudied in neuro-oncology. This study explores if patient factors impact the frequency, symptomatology, and or severity of AEs associated with standard-of-care adjuvant therapy for GBM.
Methods: We retrospectively reviewed a prospectively identified database of all adult patients undergoing surgery for GBM followed by standard-of-care adjuvant therapy – concurrent temozolomide (TMZ) chemotherapy and radiotherapy, followed by TMZ cycles – at an academic, tertiary, and quaternary care institution. Demographic (age, sex, race/ethnicity), tumor (pathology, location), adjuvant therapy (regimen, timing, AE prophylaxis), and AE history (incidence, symptoms, severity, clinical response) were collected. Descriptive statistics, bivariate analyses, and multivariable logistic regression were conducted to identify associations between patient demographics, tumor characteristics, and adjuvant therapy variables and AE incidence, symptomatology, severity, and impact on adjuvant therapy course.
Results: 38% of all patients experienced at least one AE, most commonly during the first or second cycle (mean: 1.8). Females were more likely to experience an AE (p = 0.0385); however, age or race/ethnicity did not impact incidence. Of patients with an AE, 47% reported symptoms necessitating a delayed, reduced, or discontinued TMZ regimen. Age and sex did not moderate disruptions in ; however, Black patients were significantly more likely to have a disruption in their TMZ regimen than Asian, Hispanic/Latino, and White patients (p = 0.0653, p = 0.567, p = 0.203). Patients endorsed similar AEs across demographics. Hematological AEs (59%) were both the most common and most severe AEs; more prevalent than gastrointestinal, fatigue, allergic, and neurological AEs (p<0.001 for all comparisons).
Conclusion: Demographic factors, particularly sex and race, influence the incidence and impact of TMZ-associated adverse effects in GBM patients. Of note, Black patients were significantly more likely to have disrupted TMZ regimens. Future study can explore whether Black patients’ heightened risk of TMZ disruption is due to increased susceptibility to chemotherapy-related AEs or disparate symptom management. Understanding the contributors to and predictors of adjuvant therapy-related symptom burden is critical to reducing toxicity-related treatment interruptions and improving equity in GBM outcomes.
Racial and Socioeconomic Disparities in Ectopic Pregnancy Management at a Public Safety-Net Hospital
Authors: Ky’Tavia Stafford-Carreker, MS3 (1,3), Margaret English, MD (2), Jamie Woodley, MD (2), Nuriya Robinson, MD (2), Jennefer Russo MD (2)
Affiliations: (1) UCLA David Geffen School of Medicine, (2) Department of Obstetrics and Gynecology, UCLA – Harbor-UCLA Medical Center, (3) Charles R. Drew University of Medicine and Science
Introduction: Ectopic pregnancy is a serious condition where a fertilized egg implants outside the uterus, most often in the fallopian tube. Without prompt treatment, it can rupture and lead to life-threatening hemorrhage. It remains a leading cause of first-trimester maternal mortality. Most patients present to the ED with abdominal pain, vaginal bleeding, or syncope. This study aims to assess the association between race, insurance status, and the management of ectopic pregnancy at Harbor-UCLA, a high-volume safety-net hospital serving majority Underrepresented in Medicine (UIM) populations, where delayed care can increase complications and mortality.
Methods: We conducted a retrospective chart review of 39 patients diagnosed with ectopic pregnancy at Harbor-UCLA Medical Center from January 2020 to December 2022 under IRB approval #22-001671. We collected demographic data (race/ethnicity, insurance), clinical presentation (symptoms, β-hCG, imaging), treatment type (methotrexate vs. surgery), diagnostic delays, morbidity, and documented social determinants of health (SDOH). ACOG and institutional algorithms assessed treatment eligibility based on hemodynamic stability, β-hCG levels, ultrasound findings, and contraindications. Descriptive statistics and chi-square tests were used. Logistic regression is planned to adjust for confounders.
Results: A preliminary analysis of 39 charts revealed racial and insurance-based disparities in EP care. Black and Latinx patients more frequently presented with signs of rupture and higher β-hCG levels. They were more likely to undergo surgical management than white patients, even when eligible for methotrexate. Medi-Cal patients were also less likely to receive methotrexate than those with private insurance. Limited documentation of SDOH and delayed recognition may contribute to these inequities. Multivariate analysis is underway to evaluate whether disparities persist after adjusting for clinical and structural factors.
Conclusion: Our findings highlight disparities in ectopic pregnancy care among historically excluded populations at a public hospital. Even when meeting the criteria for medical management, Black and Latinx patients were more likely to undergo surgery. These trends reflect broader systemic barriers in reproductive care. Improving early diagnosis, consistent use of treatment algorithms, and robust SDOH screening in the ED and clinic settings may help reduce preventable complications and advance equity in early pregnancy outcomes.
Enhancing Interest and Confidence in Health Careers through Mentorship and Health Curriculum Development at an Urban Underserved High School
Authors: Andy Chung, MS3 (1), Jyoti Puvvula, MD (2)
Affiliations: (1) Charles R. Drew/UCLA David Geffen School of Medicine; (2) Department of Family Medicine and Community Health, David Geffen School of Medicine at UCLA
Introduction: Early exposure and mentorship play a critical role in shaping students’ pursuit of healthcare careers, yet youth from underserved communities often lack these opportunities. Gardena High School, an urban public school in South Los Angeles, serves a student body that is 93% socioeconomically disadvantaged. This project implemented a structured mentorship and hands-on health curriculum to increase interest in medical careers, build confidence in higher education pathways, and provide meaningful experiential learning to inspire career exploration and reduce barriers.
Methods: A structured health curriculum was implemented for 57 high school juniors and seniors enrolled in sports medicine and athletic training pathways. Weekly sessions included hands-on activities (e.g., vital signs, CPR, injury prevention, anatomy, suturing), healthcare career exploration (medicine, EMS, allied health), and individualized mentorship. A baseline survey assessed demographics, interests, perceived barriers, and confidence in health-related skills. Pre- and post-surveys using Likert scales and open-ended responses measured changes in healthcare interest, college and career confidence, skill proficiency, and perceived representation. Ongoing reflections and a longitudinal post-program survey will evaluate shifts in self-efficacy, career goals, and sense of belonging in healthcare.
Results: At baseline, 42% (24/57) of students expressed interest in healthcare careers, primarily nursing and medicine. Top reported barriers included financial constraints (49%), academic challenges in STEM (25%), and lack of mentorship (21%). Confidence in first-aid skills was moderate (mean 3.8/5), while understanding of healthcare career pathways was lower (mean 2.7/5). Preliminary qualitative feedback highlighted strong enthusiasm for hands-on activities (e.g., CPR, suturing), mentorship from diverse role models, and support with college preparation.
Conclusion: Preliminary findings suggest that structured mentorship and experiential health curricula can increase interest, confidence, and perceived representation in healthcare among underserved students. Continued post-program evaluation will assess long-term impacts on students’ career aspirations and identity formation in health professions. Overall, this educational approach offers a promising strategy to diversify the future healthcare workforce and promote equity in underserved communities.
Identifying the Historical Origins of Systemic Racial Bias in the Treatment of Keloids among Patients of African Descent
Authors: Kushagra Tewari (1), Lucas Karamanoukian (2), Levon Karamanoukian (2), Raffy Karamanoukian, MD (3), Condessa Curley, MD, MPH (4, 5), Manuel Mendoza, MD (6)
Affiliations: (1) David Geffen School of Medicine, UCLA, (2) Brentwood High School, (3) Kare Plastic Surgery, (4) Martin Luther King Jr Center for Public Health, (5) Los Angeles County Department of Public Health, (6) Department of Family Medicine, UCLA Health Toluca Lake
Introduction: In the age of modern medicine, it is extremely important to recognize and erase systemic racial bias, especially if the patterned use of medical bias affects patient care. The erroneous notion that keloid scars are associated with ‘black skin’ is deeply-rooted in historical medical literature from the late 19th and early 20th centuries and embedded in our current medical literature. Our goal is to explore these historical texts to identify the origins of racial bias associated with keloid scar formation. In doing so, we can address these false narratives so that minority populations are not marginalized in our modern healthcare system.
Methods: We performed a historical exploration of extant medical texts from the 19th and 20th centuries to identify archetypal references to keloids and darker skin.
Results: Three books, including The Surgical Pecularities of the American Negro [sic, 1896], The Journal of Cutaneous Diseases, Including Syphilis (1908), and the Journal of the Royal Army Medical Corps (1945) reinforce and legitimize stereotypes that keloid scars are predominately associated with ‘black skin.’ These stereotypes are further promulgated by references to tribal scarification among Africans “in the old slave days;” and notes regarding “...lash strokes on the body…as permanent and indelible evidence of the punishment of the slave.”
Conclusion: Historical narratives describe keloids as a benign skin disease that predominantly occurs in patients of African descent. Persistence of these early stereotypes in medicine contribute to the marginalization of minority patients as poor surgical candidates due to high scar risk. The origins of such historical narratives underscore that references to African tribal scars and scars from slave-torture may have contributed to false associations that 1) keloid scarring is associated with ‘black skin’ and 2) patients of African descent may be poor candidates for elective surgery because of scar risk.
-
Built Outside, Broken Inside: Anabolic Steroid-Induced Cardiomyopathy in a 45-year-old Male
Authors: Cameron Carlisle, BS (1,2), Syed Hasan, MD (1), Harnek Singh, MD (1)
Affiliations: UCLA-Rio Bravo Family Medicine (1); Ross University School of Medicine (2)
Introduction: Anabolic-androgenic steroids (AAS) are widely used for muscle enhancement, particularly among athletes and bodybuilders, with an estimated 3-4 million users in the United States. Despite their popularity, AAS misuse poses significant cardiovascular risks, including cardiomyopathy, heart failure, and arrhythmias. Up to 30% of chronic users develop left ventricular hypertrophy (LVH), but long-term cardiac outcomes remain poorly defined. We present a case of a 45-year-old male with chronic AAS misuse, severe LVH, heart failure, and atrial flutter, highlighting the need for clinical awareness.
Methods: A 45-year-old male with a history of hypertension, type 2 diabetes mellitus, alcohol use disorder, and prior heart failure presented with altered mental status, dyspnea, fatigue, and palpitations. He reported chronic anabolic steroid use (300 cc daily for three years) to maintain physical performance and admitted heavy alcohol consumption. On exam, he had tachycardia, hypertension, bilateral crackles, and +2 pitting edema. Electrocardiogram showed atypical atrial flutter (145 bpm). Echocardiography revealed an LVEF of 35-40% with severe concentric LVH, low-flow, low-gradient aortic stenosis, and no thrombus. Elevated testosterone (4754 ng/dL) and estrogen levels were noted. The diagnosis of AAS-induced cardiomyopathy was supported by the combination of severe LVH, reduced EF, and prolonged high-dose AAS use. Management included guideline-directed medical therapy (GDMT) for heart failure, anticoagulation for atrial flutter, and tapering testosterone. The patient expressed a willingness to reduce steroid use and alcohol consumption.
Discussion: AAS misuse can cause cardiomyopathy through myocardial toxicity, increased afterload, oxidative stress, and endothelial dysfunction, leading to LVH, fibrosis, impaired function, heart failure, and arrhythmias. This case is unique due to severe concentric LVH and reduced LVEF (35-40%) from prolonged high-dose AAS use, compounded by hypertension and alcohol abuse. Severe concentric LVH linked to AAS is uncommon, making this presentation significant. Management focused on GDMT for heart failure, arrhythmia control, and AAS cessation. Idiopathic or hypertensive cardiomyopathy were considered, but the link to AAS use guided decisions. This case highlights the need to assess AAS use in patients with unexplained cardiomyopathy. Further studies are needed to improve management and outcomes.
Chronic Right Arm Swelling in a Diabetic Weightlifter: An Unusual Etiology
Authors: Cameron Carlisle, MS IV (1,2), Lovedip Kooner, MD (1), Gagan Kooner, MD (1), Alex Casey, DO (1), Harnek Singh, MD (1)
Affiliations: (1) UCLA-Rio Bravo Family Medicine Residency Program; (2) Ross University School of Medicine
Introduction: Pyomyositis is typically caused by Staphylococcus aureus, presenting with muscle pain, swelling, and systemic symptoms. In immunocompromised individuals, atypical infections, including fungal infections, can mimic pyomyositis. Coccidioidomycosis, caused by Coccidioides species, is endemic to the western US and can disseminate in at-risk populations, particularly those with diabetes. This unique case highlights disseminated coccidioidomycosis presenting as cellulitis and pyomyositis in a 50-year-old diabetic athlete, emphasizing the importance of considering fungal infections in atypical cases.
Methods: A 50-year-old male with non-insulin-dependent diabetes and a history of strenuous weightlifting presented with a 10-day history of progressive right arm pain and swelling. He had previously been treated for presumed cellulitis with oral antibiotics, but symptoms worsened. On presentation in the emergency department, he was tachycardic and hypertensive. Laboratory results showed elevated lactic acid of 2.4 mmol/L, WBC count of 10.1 × 10³/µL with 27% bandemia. Imaging revealed subcutaneous edema in the right arm and reticulonodular lung opacities. He was admitted for presumed cellulitis, sepsis, and possible pneumonia, and started on IV Zosyn. Infectious disease confirmed disseminated coccidioidomycosis via positive IgM and fungal wound cultures. He received fluconazole 800 mg daily for one week, then 400 mg daily, with incision and drainage of abscesses by orthopedic surgery. Liver function tests and serologies remained stable, and repeat CT scans showed no progression of pulmonary nodules. He regained strength with physical therapy and plans to resume weightlifting soon.
Discussion: This case emphasizes the importance of considering fungal pathogens in patients from endemic regions with atypical or refractory soft tissue infections. Disseminated coccidioidomycosis can mimic bacterial conditions like cellulitis or pyomyositis. The patient’s uncontrolled diabetes and strenuous weightlifting contributed to immunosuppression and localized tissue stress, facilitating fungal dissemination. Early recognition via serologic testing and imaging was essential. A multidisciplinary approach, including infectious disease and orthopedics, ensured optimal management. This case highlights the need for a broad differential diagnosis and tailored treatment based on regional epidemiology and patient risk factors, especially in diabetic individuals in endemic areas.
Dermatomyositis management in resource-limited areas and developing guidelines for primary care physicians
Authors: Kim Duong MS III(1), Anna Mikami MS III(2), Cameron Carlisle MS IV(4), Syed Hasan MD PGY1(3), David Song MD PGY2(3), Mariano Rubio Garcia MD PGY1(3), Harnek Singh MD(3)
Affiliations: (1) Western University of Health Sciences, Pomona, CA, US; (2) Western University of Health Sciences, Lebanon, OR, US; (3) UCLA-Rio Bravo Family Medicine Residency Program; (4) Ross University School of Medicine
Introduction: Dermatomyositis (DM) is a rare inflammatory myopathy characterized by proximal muscle weakness and distinct skin involvement, with an estimated incidence of 1.1 per 100,000 person-years in the United States. We present a 68-year-old female with bilateral arm weakness and pain, facial numbness, an erythematous pruritic rash, and dysphagia. Despite a history strongly suggesting DM, official diagnosis was complex due to the absence of local specialists, stressing the importance of management of rare diseases in resource-limited areas and developing interim guidelines for primary care providers.
Methods: A 68-year-old female with hyperlipidemia, prediabetes, and osteoporosis presented with worsening arm weakness and left facial numbness. She reported two months of shoulder myalgia and myopathy, an erythematous pruritic rash, night fevers, and dysphagia. Outpatient workup revealed elevated creatine kinase levels and aldolase level to 8.7, and positive ANA with titer 1:1280. Anti-Jo-1, anti-dsDNA, and anti-Sm antibodies were negative.
Initial NIHSS score was 1 for mild-to-moderate sensory loss. Stroke work-up was unremarkable. MRI showed extensive shoulder muscle myositis. Inpatient labs showed: AST 96, CRP 1.15, creatine kinase 833, ESR 34. On exam, patient had erythematous patches on bilateral arms, periungual telangiectasia, holster sign, and heliotrope rash.
This is a case of a patient who presented with facial numbness, concerning for a transient ischemic attack, along with chronic symmetric myopathy, dysphagia, and a rash, suggesting dermatomyositis. Urgent referrals were placed to rheumatology and general surgery however, the closest specialist was located over 100 miles away.
Discussion: Dermatomyositis is an autoimmune condition associated with a six-fold increased risk of malignancy, making early diagnosis essential for identifying potential underlying cancers. The scarcity of local rheumatologists with expertise in dermatomyositis management highlights the challenges of treating this disease in resource-limited areas such as the Central Valley. In the meantime, primary care physicians should remain vigilant with age-appropriate cancer screenings and have established guidelines for provisional diagnostic workups and treatment. The presentation of dermatomyositis with dysphagia is atypical and may signal advanced disease. Such patients would benefit from expedited care to prevent further disease progression and deterioration in quality of life.
Delayed Presentation of a Chronic Type VI Acromioclavicular Joint Separation in an Unhoused Individual
Authors: Simon P. Lalehzarian, MHA MS (1, 2), Leopoldo Hartmann Manrique, MD (1), Harnek Singh, MD (1)
Affiliations: (1) UCLA-Rio Bravo Family Medicine Residency Program; (2) American University of the Caribbean School of Medicine
Introduction: Acromioclavicular (AC) joint injuries account for more than 40% of shoulder injuries with nearly 10% resulting from collision related incidents. While mild injuries carry a favorable prognosis, severe injuries can lead to significant loss of strength and function. To make matters worse, unhoused individuals are affected by musculoskeletal conditions at a higher rate due to a higher prevalence of contributing factors such as histories of physical/sexual abuse and substance abuse disorders. Here, we present a case of an unhoused gentleman who suffered a rare Type VI AC joint separation.
Methods: An elderly unhoused male presented with left shoulder pain a few years after being assaulted by another unhoused individual near his encampment. Patient states he remembers being hit from behind and stretching out his arm to catch himself. Since the injury, the patient has had pain radiating to his neck that worsens with movement and when he tries to sleep on the affected shoulder. On examination, the patient has an obvious visible deformity with significant tenderness to palpation at the AC joint and lateral clavicle. He has a reduced range of motion secondary to pain. Special examinations elicited a positive O’Brien’s test and crossbody adduction test. Bilateral shoulder x-rays were obtained with the left shoulder demonstrating significant displacement from the top of the coracoid to the bottom of the clavicle. Using the Rockwood classification, patient was diagnosed with a Type VI AC joint separation. Patient was then referred to an orthopedic sports medicine specialist for possibility of surgical treatment and for routine primary care follow-up through Street Medicine.
Discussion: Unhoused individuals are often exposed to harsh living situations which increase their vulnerability to musculoskeletal injuries. Factors such as substance abuse and mental illness predispose unhoused individuals to injury and assault while competing priorities such as securing food or shelter make them more likely to forego medical care. As a result, unhoused individuals often have inadequate access to care and rely on emergency departments to treat their injuries. These findings have important implications and highlight the need for evidence-based interventions and increased follow-up. Targeted efforts and better tracking of follow-up could improve health outcomes for unhoused individuals and reduce the need for costly late-stage interventions by providing early and more consistent care.
-
Disparities in Pediatric Orthopedic Care in Los Angeles: An Analysis of Wait Times for Physical Therapy
Authors: Shane Hervey, MD, Ashley Lopez, BS, My Nguyen, BS, Alexander Soto, MD MPH, Emily M. Miller, MD, Calvin Duffaut, MD
Affiliations: University of California, Los Angeles, Department of Family Medicine, Division of Sports Medicine
Introduction: This study examines disparities in pediatric musculoskeletal care, comparing wait times for physical therapy (PT) across clinical sites using the Social Vulnerability Index (SVI), ethnicity, race, language, and insurance type. It aims to identify inequities and inform interventions to improve access.
Methods: This retrospective cohort study analyzes medical records to calculate wait times from referral to the first PT session. Pediatric patients aged 8-17 seen in orthopedic clinics from July 1, 2019, to June 30, 2024, were included. Data management and analysis, using R-Studio, involve univariate analysis, a correlation test, and a power analysis.
Results: Of 252 records, the median PT wait time was 18.9 days for patients identifying as African-American, 19.9 for Caucasian, and 19.5 for Other Identified Groups. No statistically significant difference was observed across races (p = 0.76). Median PT wait time was 18 days for Hispanic/Latino patients, 19.9 for non-Hispanic/Latino patients, and 21.5 for Other Identified Ethnicities with no statistically significant difference observed (p = 0.34). Median PT wait time was 20.0 days for English speakers, 17.3 for Spanish, 18.6 for Korean, and 34.7 for Japanese with no statistically significant difference observed (p = 0.37). Median PT wait times were 22 days with Commercial insurance, 19 with Government, and 64.1 with Other coverage with no statistically significant difference observed (p = 0.92).
Conclusion: No statistically significant differences were observed across race, ethnicity, primary language, or insurance coverage. These findings suggest that these factors may not independently influence PT wait times within this dataset. Future research with additional variables, such as socioeconomic status using SVI data, may provide further insights into disparities in physical therapy access and approval processes.
Academic-Community Partnerships to Improve Acute Pediatric TBI Management
Authors: Anisha Patel, DO, Alexander Kertzner, MD PhD, Ngoc Duong, DO, Cyrus Nensey, MD, Howard Jen, MD MS, Richard Kang, MD
Affiliations: Dignity Health - Northridge Medical Center
Introduction: Over 500,000 pediatric traumatic brain injury visits present to general emergency departments and community hospitals annually. Experts have raised concern of pediatric emergency preparedness and variation in the standard of care between community hospitals and academic centers, while also raising awareness of the risks associated with exposing children to ionizing radiation. This study seeks to help inform whether academic-community partnerships are a model for improving quality of care and CT scan usage in pediatrics with TBI who are initially evaluated in a community hospital setting.
Methods: In 2010, Northridge Hospital Medical Center, a not-for-profit community hospital, was designated a pediatric trauma center, establishing a collaborative relationship with academic institution University of California Los Angeles. In January 2020, the partnership evolved with UCLA as pediatric trauma surgeons became consultants with the primary trauma team, thereby increasing the number of clinicians involved in patient care. This retrospective medical chart review examines data collected from 2016 to 2024 to assess changes in CT scan utilization and adherence to the PECARN rule following these changes. PECARN is a validated clinical decision tool for excluding unnecessary CT imaging for patients under 18 years old at low risk of having clinically significant TBI.
Results: Final data analysis is currently pending. Demographic and clinical variables will be summarized using descriptive statistics. Comparative analysis will be performed to evaluate changes in CT scan utilization between January 2016 to December 2019 and January 2020 to May 2024 when the nature of the academic-community collaboration changed.
Conclusion: Tailored clinical evaluation remains essential for providing timely and effective management while minimizing unnecessary risks, particularly in community hospital settings. Preliminary analysis suggests that an academic-community collaborative model may enhance access to high-quality care for TBI patients and be a means of integrating evidence-based practice in community hospitals.
Improving the PGY-1 Experience with Intern Lecture Series Curriculum at the Harbor UCLA Family Medicine Program
Authors: Camila Salazar, DO; Carina Franco, MD; Juan Carlos Sanabria, DO; Mahuya Barua, MD; Jyotti Puvvula, MD/MPH; Fathima Nazarkhan, MD; Karen Olmos, MD/MPH
Affiliations: Harbor-UCLA Family Medicine (HUCLA FM) Residency Program
Introduction: Lecture-based learning is a tradition in didactics; however, the “engaged classroom” format has improved knowledge retention. A flipped classroom, where the instructor becomes a moderator instead of a performer, is an example of an “engaged classroom” by encouraging learners to be active participants. HUCLA FM’s Intern Lecture Series (ILS) entails 45 minutes of protected learning time once a week to cover core curricular topics. The study aims to ascertain the PGY-1s preferred mode of delivery of core educational content to enhance learning and improve learning satisfaction.
Methods: The study is a cross-sectional descriptive design based at HUCLA FM. After 6 months of participation in traditional ILS sessions, PGY-1s in the Class of 2027 were given a survey to better characterize their satisfaction and learning. PGY-1s will be offered one ILS session using a flipped classroom format. A post-intervention survey will assess learner satisfaction and retention of knowledge. The statistical method is descriptive, summarizing data using indexes.
Results: 11 out of the 12 PGY-1s completed the pre-intervention survey. Nearly a third would prefer active engagement through questions and discussions. 9% prefer a mix of case-based and active learning. None wanted passive lectures. On a scale of 1 to 5, with “1” indicating not satisfied at all and “5” indicating the highest level of satisfaction with the current format, the majority (64%, N=7) indicated that they were neutral. 18% (N= 2) were very satisfied, and 9% (N= 1) were extremely satisfied. 9% (N =1) were not satisfied. 73% indicated that memorable sessions had practical application. 55% wanted more case/question-based content, and 27% wanted interaction, such as games. 27% wanted key takeaway points at the end of the lecture. Final results will include post-intervention survey results.
Conclusion: ILS is one of the few protected spaces for PGY-1s to learn core content. The goal is to assess the efficacy of PGY-1 learning and satisfaction with ILS by exploring ways to improve overall learning. Preliminary data shows room for further growth in how the educational content may be delivered using cases, questions, games, and discussion. We will conduct a session incorporating the preferred learning formats in the pre-intervention survey. Future goals include sharing the results with faculty and senior residents, as well as conducting workshops on content delivery.
Climate Extremes and Patient Behavior: Investigating the Impact of Extreme Heat and Rain on No-Show Rates at Dignity Health Northridge Family Medicine Clinic
Authors: Catherine Khasho, DO and Christopher Kuhlman, MD
Affiliations: Dignity Health - Northridge Medical Center
Introduction: Physicians at our clinic have observed a perceived correlation between weather conditions such as high heat or rainfall and an increase in patient no-show rates. However, this relationship has not been studied. Our project aimed to determine if such a correlation exists. If so, it could lead to actionable strategies for anticipating no-shows. In a clinic that is often overbooked and faces challenges in scheduling timely follow-up appointments, the ability to predict no-shows based on weather patterns could allow for more efficient scheduling.
Methods: In this retrospective study, data was collected from two primary sources. First, The Weather Channel (weather.com), specifically identifying dates in Northridge, CA from January 2024 to December 2024 when temperatures reached 90°F or higher, or when any amount of rain occurred. Second, data on patient arrivals and no-shows was collected from our clinic’s scheduling portal for the same dates. Based on the percentage of arrivals and no shows on extreme weather and normal weather days, expected frequencies were calculated and then used to calculate the chi square test and compare it to the critical value which was obtained from a chi square distribution table based on degree of freedom of 1 and significance level of 0.05.
Results: We analyzed one calendar year worth of data regarding Northridge, CA weather conditions and no-show rates in our clinic. The chi square value was 0.104 which is less than the critical value 3.841. Based on this, we fail to reject the null hypothesis: No correlation exists between extreme weather conditions (defined as temps exceeding 90F or any amount of rainfall) and no-show rates at the clinic. Meaning, there is not enough evidence in our sample data to conclude that the null hypothesis is false. This does not necessarily mean the null is true, just that the data we have does not provide strong enough evidence to support the alternative hypothesis: A positive correlation exists between days with temperatures exceeding 90F or any amount of rainfall and higher no-show rates at the clinic.
Conclusion: Despite a perceived correlation between weather conditions and an increase in patient no-show rates, we found no significant association in 2024. Limitations include small sample size and utilizing clinic wide no-show rates rather than only the no-show rates of our physicians who themselves perceive a correlation. Future research should assess if a correlation exists between high temperature and rainfall separately. While our study did not find a significant correlation, it provides valuable insight into the importance of rigorous data analysis in testing perceived clinical trends.
Impact of Urology Specialist Lecture on PSA Screening Practices Among Family Medicine Residents
Authors: Christina Nguyen, DO, Sara Larsen, MD, Kathleen Dor, MD
Affiliations: Department of Family Medicine at Kaiser Permanente Woodland Hills
Introduction: Prostate cancer is the second leading cause of cancer-related deaths in men, yet its screening remains controversial. While PSA testing can detect cancer early, conflicting guidelines have led to uncertainty among clinicians. The USPSTF and AUA provide differing recommendations, leaving family medicine residents navigating evolving practices. It is unclear how educational interventions impact their screening behaviors. This study examines whether a urology specialist lecture influences PSA screening rates among residents, aiming to identify gaps in knowledge and improve adherence to current guidelines.
Methods: This retrospective study was conducted at Kaiser Permanente Woodland Hills to assess the impact of a urologist lecture on PSA screening practices. Medical records of men aged 55-69 seen by family medicine residents between August 9th and December 10th, 2024 were reviewed. Patients with prior PSA testing within two years or a history of prostate cancer were excluded. The intervention was a lecture covering PSA screening guidelines. The primary outcome was the change in PSA ordering rates, including patients who declined screening after discussion, before and after the lecture. The ordering rates were compared to those of other family medicine residents who were unable to attend the lecture. The data was analyzed using a paired t-test to compare pre-lecture to post-lecture ordering rates.
Results: A total of 144 men were seen by residents who attended the lecture, but 91 had prior PSA screening in the past 2 years and 4 had a history of prostate cancer, leaving 49 eligible patients. Among residents who did not attend, 100 men were seen, but 50 had prior PSA screening in the past 2 years and 6 had a history of prostate cancer, leaving 44 eligible patients. Residents who did not see any eligible patients before or after the lecture were excluded from analysis. A two-tailed paired t-test showed PSA ordering rates increased from 15.0% to 66.1% among lecture attendees (p = 0.0471), while non-attendees increased from 15.7% to 22.2% (p = 0.2875), indicating the lecture significantly improved screening adherence.
Conclusion: A urologist lecture significantly improved PSA screening rates among family medicine residents, with ordering rates increasing from 15.0% to 66.1% among attendees, while non-attendees showed a smaller, nonsignificant increase from 15.7% to 22.2%. The initially low screening rates highlight the need for emphasis on PSA screening guidelines in training to ensure optimal patient care, and that targeted educational interventions can enhance adherence to prostate cancer screening guidelines. Further research is needed to assess long-term knowledge retention.
-
Winging It—A Rare Case of Lateral Scapular Winging
Authors: Alan Z. Grusky, MD (1) and Calvin J. Duffaut, MD (1)(2)(3)
Affiliations: (1) University of California, Los Angeles (UCLA) Department of Family Medicine; (2) UCLA Department of Orthopaedic Surgery; (3) UCLA Division of Sports Medicine
Introduction: A 34-year-old left-hand dominant male with medical history of atrial fibrillation, epilepsy, and migraines presented with chronic left anterior shoulder pain and subacute loss of shoulder range of motion. His presentation later evolved to include shoulder asymmetry. He was later diagnosed with Parsonage-Turner Syndrome, a rare, idiopathic peripheral neuropathy associated with inflammation of the brachial plexus. It is an under-recognized cause of shoulder pain, weakness, loss of ROM, and/or scapular winging that should be on the differential diagnosis for atraumatic shoulder pain.
Methods: Patient's pain started approximately two years prior to presentation while weightlifting without any acute inciting event/trauma. Patient took several months off from lifting and pain subsequently resolved. About three months prior to presentation, patient resumed weightlifting but noticed shoulder asymmetry. When seen in clinic, patient endorsed reduction in left shoulder ROM and was unable to participate in certain activities such as kayaking. Denied numbness or tingling in neck or upper extremity. No fevers, chills, or systemic symptoms. Denied any prior injuries or surgeries.
Physical exam: + left lateral scapular winging and atrophy of the left trapezius muscle, full and symmetric ROM and strength of the neck/shoulders. + scapular dyskinesia. Negative special testing for rotator cuff, impingement, biceps, and labral pathology.
Imaging: Left shoulder XR: Negative; Cervical spine XR: Negative; EMG: evidence of spinal accessory neuropathy of the left upper extremity; MRI cervical spine: mild-moderate left foraminal stenosis at C5-C6 and C7-C8.
Discussion: Parsonage-Turner Syndrome is a rare, idiopathic peripheral neuropathy associated with inflammation of the brachial plexus. It is an under-recognized cause of shoulder pain, weakness, loss of ROM, and/or scapular winging. The pathophysiology is poorly understood but is thought to be immune-mediated. Classically, it presents with severe, acute pain followed by weakness, most commonly involving the suprascapular, long thoracic, and anterior interosseous nerves. As evidenced by this case, there is significant variability in the natural history and presentation. Clinicians should maintain a low threshold to obtain EMG for diagnosis of PTS when suspicion is high even in the absence of risk factors.
A Rare Co-Recurrence of Both Primary and Secondary PV in an Elderly Patient with COPD
Authors: Alejandra S. Lopez, MD (1); Verna Marquez, MD APD (2); Harnek Singh, MD (2); Carol Stewart-Hayostek, MD PD (2)
Affiliations: (1) Rio Bravo Family Medicine Residency Program, Clinica Sierra Vista, Kern Medical Center, Sierra View Medical Center; (2) Rio Bravo Family Medicine Residency Program, Clinica Sierra Vista, Kern Medical Center
Introduction: Polycythemia vera (PV) is a BCR::ABL1-negative myeloproliferative neoplasm characterized by an increased red blood cell (RBC) mass and increased risk for thrombosis, leukemic transformation, and/or myelofibrosis (MF). Almost all patients with primary PV have a mutation of the JAK 2 gene. Secondary polycythemia is caused by high EPO in the setting of chronic hypoxia or an EPO-secreting tumor. It is important to rule out primary PV prior to considering secondary polycythemia as the diagnosis as it changes risk stratification and management.
Methods: A 78-year-old female with PMH of severe COPD (2-3L home O2) and former chronic smoking (40+ pack years), was referred to the clinic for incidental polycythemia. Labs revealed hemoglobin of 19.3g/dL, hematocrit of 63%, and platelets 783,000/mcL. Peripheral blood smear obtained depicted polycythemia with microcytosis, anisocytosis, and thrombocytosis. Testing for JAK2 V617 mutation was positive, and the patient was diagnosed with primary polycythemia vera. Patient was treated with low-dose aspirin, hydroxyurea, and weekly therapeutic phlebotomy with a hematocrit goal of 50% instead of 45% for permissive polycythemia in the setting of COPD. Patient’s hemoglobin and hematocrit levels improved to goal and continued through day 77. After the 77th day, she was lost to follow up. Six months later, the patient presented to the ED for acute COPD exacerbation. Her hemoglobin was 16.0 and hematocrit was 55.7 at that time because of non-compliance with medications as previously prescribed. She was restarted on hydroxyurea and again lost to follow-up after discharge.
Discussion: Polycythemia vera presents a challenge for many physicians. The extensive symptomatology can be mistaken for other conditions. This patient had acute hypoxic respiratory failure secondary to COPD exacerbation with underlying polycythemia vera. PV's incidence is 0.84 and prevalence rate is 22 cases per 100,000. With prior history of COPD, her erythrocytosis was initially thought to be from secondary polycythemia. During hematology referral, patient was discovered to have the JAK2 V617F mutation on genetic testing, confirming primary PV with a secondary component. Clinicians must do the appropriate labs, genetic testing, and blood smear to confirm primary PV versus secondary polycythemia for risk stratification and proper treatment, including phlebotomy, aspirin, and cardiac risk reduction.
Unmasking the Hidden Threat: Euglycemic Diabetic Ketoacidosis in a Type 2 Diabetic on Sodium-Glucose-Transporter-2 Inhibitor with Suspected Sepsis – A Case Report
Authors: Belonwu Valentine Okafor, MD, Jose-Corea Gonzalez, MD, Arthur Peter Yagubyan,MD
Affiliations: Department of Family Medicine at Mission Community Hospital
Introduction: Euglycemic diabetic ketoacidosis (EuDKA) is a rare life-threatening condition often underdiagnosed due to the absence of significant hyperglycemia. It accounts for approximately 2-3% of all DKA cases. Its incidence has risen with the increased use of SGLT-2 inhibitors. We present a 46-year-old female with type 2 diabetes on Farxiga who developed euglycemic DKA, masked by possible sepsis from cellulitis. This case highlights the need for clinical vigilance on SGLT-2 inhibitor users presenting with atypical symptoms and metabolic acidosis.
Methods: We report a case of a 46-year-old female with type 2 diabetes on SGLT-2 inhibitor (Farxiga), who presented with a three-week history of left hallux pain and swelling after pedicure. The swelling progressed to a pustular lesion that improved partially with dicloxacillin. However, the patient experienced progressive left foot and leg swelling with pain, vomiting, poor oral intake, abdominal pain, and fatigue. Upon evaluation, SIRS criteria were met (WBC 22, HR 118) with cellulitis as a source. Initial management with isotonic fluid therapy and antibiotics alone led to worsening systemic symptoms. Further evaluation revealed significant metabolic acidosis (bicarbonate 7 mEq/L, pH 6.97, anion gap 25) with 3+ ketonuria, small serum ketones, and near-normal blood glucose level of 179 mg/dL. Other pertinent labs were negative utox, negative bHCG, Etoh <10, and Lactate 2.1. This raised suspicion for EuDKA. Swift intervention with dextrose containing fluid, bicarbonate infusion, insulin infusion, and supportive care, led to stabilization and clinical improvement.
Discussion: EuDKA is a rare but serious complication of SGLT-2 inhibitors (<0.2% incidence, 1.57% fatality). Glycosuria-induced dehydration and stress hormone upregulation drive ketogenesis, with poor intake and infection as additional triggers. Atypical presentation complicates diagnosis, requiring exclusion of other causes of anion-gap metabolic acidosis. Leukocytosis and tachycardia may reflect infection, hemoconcentration, or stress. Our case contributes to the growing understanding of SGLT-2 inhibitor- induced EuDKA. It highlights the need for high suspicion of EuDKA in SGLT-2 inhibitor users with metabolic acidosis. Identifying triggers and mimickers like sepsis is crucial, though further research is needed to clarify if EuDKA in SGLT-2 inhibitor users can occur without additional triggers.
Conservative Management is Not Always Enough for Proximal Fifth Metatarsal Fractures
Authors: Bernadette Pendergraph, MD
Affiliations: Harbor-UCLA Medical Center
Introduction: Inversion injuries to the ankle and foot are common and include lateral ankle sprains, fifth metatarsal fractures (avulsion, Jones, and dancer), osteochondral injuries, fractures of lateral/posterior process of the talus, and fractures of the anterior process of calcaneus. This individual had a classic inversion injury with avulsion fracture of the proximal fifth metatarsal that failed immobilization leading to surgery. Careful instructions to patients about what constitutes protected weight bearing can ultimately affect success of conservative treatment.
Methods: 48-year-old-female runner complained of right lateral foot pain after awkwardly landing on 2nd base during a softball game. She initially felt a pop but continued to play. Exam showed soft tissue swelling and tenderness of the lateral ankle and proximal 5th metatarsal but no instability or tenderness at the Lisfranc joint. Xray showed a proximal fifth metatarsal fracture with 3 mm of diastasis that was treated with protected weight bearing in a walking boot. Follow up xray showed increasing diastasis so she was placed in a non-weight bearing cast for 4 wks and then a walking cast for 4 wks. Because of persistent pain and a CT showing diastasis without callus formation at the base of the fifth metatarsal consistent with non-union, she was referred to a foot/ankle surgeon and an ORIF of the fifth metatarsal fracture with bone autograft from the calcaneus was performed. Postoperatively, she was transitioned from a posterior splint to a non-weight bearing cast, followed by a walking cast, and to a shoe. She completed a home rehabilitation program and is back to running half marathons.
Discussion: Injuries to the base of the fifth metatarsal are divided into 3 zones and are predisposed to poor healing due to limited blood supply. Zone 1 fractures of the fifth metatarsal tuberosity occur when the hindfoot is forced into inversion during plantarflexion and referred to as avulsion fractures. Zone 2 fractures occur with forefoot adduction and zone 3 fractures typically occur due to repetitive microtrauma. Zone 1 fractures respond well to protected weight bearing in a hard soled shoe, walking boot or cast and progress over 4-8 weeks. Although Zone 1 fractures rarely need surgery, the degree of diastasis as well as noncompliance with activity modification led to surgical management in this athlete. Clear instructions for safe activities and driving are crucial for successful treatment.
Decreasing Hemoglobin A1c, Progress or Pathology?
Authors: Daniel Gehlbach, MD, MPH; Chai L. Arnold, MD; Gerardo Moreno, MD, MSHS, FAAFP
Affiliations: Department of Family Medicine at UCLA
Introduction: A 67-year-old female with multiple comorbidities presented to clinic for a routine follow up for chronic conditions including management of diabetes. This patient who has been seen by various residents over the years has had a declining Hemoglobin A1c. This case presents a good example of thinking twice before chalking up improvement in A1c. In addition, this case provides an example of multidisciplinary coordination of care to diagnose and treat a patient's underlying condition in a timely manner.
Methods: The patient reported subjective episodes of hypoglycemia with sugars in the 40-70's and symptomatic dizziness. She had suffered multiple falls and consequently had several emergency department visits. Through chart review, it was discovered that this patient’s HgbA1c had continued to decrease despite removing diabetes medications and no major lifestyle changes. Her A1c had previously been as high as 10% but now was 5.4%. Labs, imaging, and an e-consult to Endocrinology were placed. The diagnostic evaluation revealed elevated insulin (47.8) and c-peptide (11.2) in the presence of hypoglycemia on the same lab draw. Imaging within weeks included CT and MRI scans revealing a pancreatic tail mass. Endocrinology recommended urgent surgical consultation for removal of the mass. A month later Surgical Oncology performed a distal pancreatectomy and splenectomy, with final pathology confirming an insulinoma. Post-op follow up included PCP, surgical, and Endocrinology visits. The patient has since resumed metformin for glycemic control and has had no further hypoglycemic events or falls.
Discussion: Insulinoma is a rare diagnosis that occur in 1 to 4 people per million per year, however if overlooked or missed could lead to detrimental outcomes. While insulinomas once diagnosed have a fairly straightforward algorithm for treatment, the detective work of discovering one is not always straightforward. In this case, a patient with 5+ chronic conditions with an improving A1c who presents to a busy resident-run clinic could easily have been overlooked. Due to time constraints, diabetes could easily have been viewed as improving and moved along to the next concern. The case presents an opportunity to remind us to be thorough in our history taking and stay curious about abnormal trends and symptoms.
TACO as a Challenge in the Management of a Teenager with Abnormal Uterine Bleeding in the Acute Setting
Authors: Ernesto Ricardo Ojeda, MD, Katherine Ruiz Soto, MD, Christal M Clemens, MD
Affiliations: UCLA Department of Family Medicine, Family Medicine Residency
Introduction: Abnormal uterine bleeding (AUB) causes quality of life disruptions. Treatment can be challenging if a clear etiology is not identified. In emergencies, the health history may be limited, and relevant preexisting disorders can be missed. For acute AUB, therapy can include some pharmacological/medical interventions including transfusions that carry complications, such as Transfusion associated circulatory overload (TACO). In this case report we describe a patient whose health integrity was threatened by the severity of AUB. We will discuss the challenges of treating AUB in an acute setting.
Methods: A 16-year-old female with history of Gray Platelet Syndrome (GPS) admitted for metro/menorrhagia and anemia. On admission Hgb: 4, Platelets: 52. She required continuous transfusions for several hours. During the 5th unit(U) of PRBCs she developed dyspnea, abdominal discomfort, and numbness/tingling of her lower back. Vitals were stable, unrevealing exam except nonpitting edema in extremities. She was given Benadryl, Tylenol, and Lasix with clinical improvement. Later, she felt lightheaded and had emesis. Given concern for an anaphylactic reaction she received epinephrine and albuterol. Notable labs: Blood Type O+, U Blood Type O+, Post transfusion DAT negative, no hemolysis noted on posttransfusion. Unrevealing CXR. Transfusion Medicine assessed that her reaction was most consistent with her underlying GPS with TACO. Further transfusions were infused at a rate of 3 hour/U, and patient was pre-treated with Cetirizine and Tylenol. Subsequently received additional 2 U of pRBC without complications. She was treated with IV estrogen followed by norethindrone and Loestrin on discharge.
Discussion: Severe Abnormal Uterine Bleeding management in the pediatric population represents a challenge for any experienced physician or physicians in training. This case adds an extra layer of complexity, given our patient's underlying genetic disorder. TACO presents with acute respiratory distress, tachycardia, and positive fluid balance. Early recognition is pivotal to guide management. This case serves to heighten awareness of TACO as a potential complication of blood transfusions, a common intervention inpatient. Although highlighted by the care team, further research is needed to establish a correlation between TACO and Gray Platelets Syndrome.
Unveiling Hidden Cardiac Pathology: Wolff-Parkinson-White Syndrome with Coexisting Cardiomyopathy in a Young Adult
Authors: Genevieve Tusa, DO, MPH; Amber Williams, DO
Affiliations: Dignity Health Family Medicine Residency Program at Northridge
Introduction: A 24-year-old male presented with palpitations and was diagnosed with Wolff-Parkinson-White (WPW) syndrome. Further investigation revealed coexisting cardiomyopathy with an undetermined etiology. This rare combination of electrical and structural heart disease presents a diagnostic challenge in young patients. WPW affects 1-3 in 1,000 individuals and is rarely associated with cardiomyopathy. Some studies suggest genetic mutations or ion channelopathies may link these conditions, highlighting the need for thorough evaluation in similar cases.
Methods: A 24-year-old male with no significant medical history presented with palpitations, chest pressure, and fatigue for 2–3 months. His EKG showed a widened QRS, prolonged QT, ST depressions, and inverted T-waves. Family history included cardiac disease in his grandfather. Social history was positive for marijuana use. In the ED, he was hypertensive and tachycardic, with EKG findings consistent with WPW syndrome and cardiomegaly on chest X-ray. BNP was elevated, but troponin was normal. Echocardiography revealed a reduced ejection fraction (25-30%) with global hypokinesis, dilated right atrium/ventricle, and moderate-to-severe valvular regurgitation. He underwent radiofrequency ablation of the accessory pathway, with post-procedure EKG improvement but persistent conduction delay. He was started on carvedilol, sacubitril/valsartan, spironolactone, and prescribed a LifeVest. A cardiac MRI was recommended. Six months later, no improvement in ejection fraction was noted, and the cardiomyopathy etiology remains undetermined.
Discussion: This case highlights the rare coexistence of WPW syndrome and cardiomyopathy of unknown origin, raising concerns about an underlying genetic or infiltrative process. WPW syndrome is seldom associated with cardiomyopathy, making the diagnosis particularly challenging. The persistent conduction delay in this patient further complicates the diagnosis. While rare, coexisting WPW syndrome and cardiomyopathy in young patients emphasizes the need for a comprehensive evaluation, especially in those presenting with heart failure or arrhythmic symptoms. Timely identification and management are crucial for optimal outcomes. Continuous follow-up with cardiology and strict adherence to medical therapy will be important for improving the long-term prognosis of this patient.
Case Report: Acute Glenoid Labral Tear in a Recreational Rock-Climbing Athlete
Authors: Harrison Lam MD, Brian Donohoe MD
Affiliations: UCLA Department of Family Medicine, UCLA Division of Sports Medicine
Introduction: Rock-climbing athletes are prone to shoulder injuries due to repetitive and strenuous overhead movements, causing microtrauma over time. As a result, chronic overuse injuries are quite common in this population. This case report discusses a 29-year-old male avid recreational rock climber who presented to a sports medicine clinic for left anterior shoulder pain after outdoor rock climbing, ultimately diagnosed with a complex glenoid labral tear and rotator cuff tendinosis.
Methods: The patient’s inciting injury occurred about one month prior while executing a move with his arms out wide and pulling himself upward. This resulted in a “crunching” sensation in the shoulder followed by significant pain and limitations in abduction and extension. Pertinent physical exam findings included mild TTP of the anterior/medial shoulder joint, normal strength 5/5 with rotator cuff special tests (though with pain reproduced anteriorly), and a positive apprehension test due to pain (though without laxity observed with anterior translocation). Yergason’s, Speed’s, and O’Brien’s tests were negative. XR was notable for normal alignment without obvious fracture or calcific tendinosis. MRI showed a complex tear of the glenoid labrum with mild tendinosis and low-grade partial thickness tear of the supraspinatus, mild tendinosis of the infraspinatus, moderate glenohumeral joint effusion, and moderate AC joint osteoarthrosis.
Discussion: This case demonstrates an acute presentation of a glenoid labral tear due to a strenuous climbing maneuver in an otherwise healthy young patient. Findings of rotator cuff tendinosis suggest underlying chronic stress, possibly increasing the risk of acute injury. The patient pursued non-operative treatment, including a combination of physical therapy, NSAIDs, and muscle relaxants. At follow-up 8 weeks after initiation of treatment, he reported improvement in his shoulder pain to about 70-85% of prior baseline and had begun resuming light rock climbing activity. He reported residual pain and tightness at the biceps tendon. He was advised to continue with conservative treatment, activity as tolerated, and consideration of a biceps tendon sheath corticosteroid injection in the future.
Snap, Crackle, and Popping Knee Syndrome: Diagnosing Discoid Meniscus
Authors: Jane J. Kang, DO
Affiliations: Department of Sports Medicine, Kaiser Permanente Los Angeles
Introduction: Discoid meniscus, often referred to as “popping knee syndrome,” is a congenital anomaly of the knee where the meniscus is abnormally shaped, leading to mechanical symptoms such as popping, clicking, or locking. This condition is most commonly seen in adolescents, with symptoms often presenting as knee instability or discomfort. The reported incidence of discoid lateral meniscus is ~3% to 5% in the United States. This case report highlights a teenage patient with a discoid meniscus, providing insight into clinical presentation, diagnosis, and management for this relatively rare condition.
Methods: A 16-year-old male presented with intermittent atraumatic right knee pain and “popping.” He reports multiple episodes of falls with his knee giving way and difficulty straightening his knee (transient locking). Physical examination was unremarkable except when performing McMurray’s test, which produced a significant repeatable clunk with end-range extension. It felt as though the tibiofemoral joint were shifting, raising suspicion of a structural intraarticular joint abnormality resulting in altered biomechanics.
X-ray was unremarkable, while MRI demonstrated a particle discoid lateral meniscus (DLM) with intrasubstance degeneration and horizontal tear of the posterior horn to meniscal body.
Given the meniscal pathology and persistent symptoms despite conservative treatment (NSAIDs, activity modification, and an exercise program), the patient proceeded with knee arthroscopy with partial lateral meniscectomy/saucerization vs. meniscus repair.
Postoperatively, the patient underwent a structured rehabilitation program, focusing on quadriceps strengthening and neuromuscular control.
Discussion: DLM is an often overlooked cause of atraumatic knee pain in young patients. Certain tear patterns, like the inverted-type DLM tear, may have a clear trauma history, but lack characteristic MRI findings, increasing risk of misdiagnosis. Given its variable presentation, early recognition is crucial to preventing long-term complications. Symptomatic DLM is linked to cartilage injury, especially in patients with prolonged symptoms (over six months), high activity levels, and an asymmetrical meniscal shape. Surgery, typically saucerization with or without meniscal repair, is often necessary. Clinicians should also be aware of potential postoperative complications like osteochondritis dissecans, which may arise from repeated chondral impaction. Postoperative rehab is key for optimizing recovery.
PM-Mito: When Mitochondria Ceases to be the Powerhouse of the Cell
Authors: Susan Li, DO, Venus Esquivel, MD, and Esther Zarecki, MD
Affiliations: Riverside University Health System/ UC Riverside
Introduction: Inclusion Body Myositis (IBM) is a progressive, debilitating and incurable disease. IBM is distinct from other muscle disorders due to asymmetric proximal and distal limb weakness, often including the fingers and wrist. Common physical findings and comorbidities such as history of stroke and diabetic neuropathy make this diagnosis challenging. Laboratory testing can be confounded by pre-existing medications and autoimmune conditions. Here we report a complex case where multiple factors challenge the ability to make the diagnosis.
Methods: A 79-year old male presented with progressive weakness of bilateral upper and lower extremities, first noted in proximal thighs 4 years ago. Over 2 years, he experienced progressive bilateral proximal and distal lower extremity weakness. He also began having difficulty holding utensils and reaching, more on the left than right, as well as intermittent dysphagia, without vocal change or speech slurring. He endorsed numbness and tingling of all limbs. On exam, he was well-appearing, on room air, and wheelchair-bound, with decreased muscle strength on all limbs and left wrist drop. Deep tendon reflexes were absent in all extremities. Work up included autoimmune labs with elevated creatine kinase, aldolase, and antinuclear antibody titer 1:1280. Myositis panel was negative. Imaging showed severe fatty atrophy and edema of the lower extremity and findings suggestive of multifocal myositis in the upper extremity. Muscle biopsy showed endomysial inflammation and mitochondrial dysfunction, but without rimmed vacuoles, indicating polymyositis with mitochondrial pathology (PM-Mito).
Discussion: The patient presented with weakness concerning for IBM. However, he also had atypical features, including late presentation in the mid-70s, male sex, and biopsy results without rimmed vacuoles, a hallmark feature of IBM. His findings are suggestive of PM-Mito. PM-Mito is on a spectrum of IBM and may represent early IBM. Mortality rates in polymyositis patients can be as high as 15% to 30% within 5 years of diagnosis, primarily due to complications related to muscle weakness, respiratory issues, or associated malignancies. The importance of early intervention to slow the inevitable disease progress is imperative. Extensive interdisciplinary management is an invaluable resource for patients and family.
-
Correlation Between Division I Collegiate Athletes’ Preseason Mental Health and Prospective Injury Rates
Authors: Connie Oh MD (1,2), Calvin J. Duffaut MD (1,2), Emily M. Miller MD (1,2), Sessen Dudek MD (2), Aurelia Nattiv MD (1,2)
Affiliations: (1) UCLA Division of Sports Medicine; (2) UCLA Department of Family Medicine
Introduction: Collegiate athletes suffer from variety of mental health related disorders. To date, there is no study that evaluates the effect of a wide variety of psychological factors on prospective injury rate in collegiate athletes. This study aims to evaluate the association between mental health concerns and prospective injury rates among Division I male and female collegiate athletes across various sports using the Counseling Center Assessment of Psychological Symptoms-62 (CCAPS-62).
Methods: Division I athletes were recruited during the 2024-2025 season. Preseason depression, generalized anxiety, social anxiety, academic fdistress, eating concerns, family distress, hostility, and substance use were measured using CCAPS-62. Injuries were recorded by athletic trainers. Injury rates were calculated by dividing the injuries by athletic exposures.
Results: 130 student athletes enrolled with 30 injuries. 12.3% athletes reported depression, 16.1% anxiety, 20% social anxiety, 17.6% academic distress, 20.8% eating disorders, 7.7% hostility, 14.6% family distress, and 7.7% substance use. Injured athletes had 1.68 times (p=0.028) more concurrent mental health concerns than non-injured athletes. Athletes with individual mental health concerns did not have significantly higher injury rates compared to those without: depression (RR=0.72; 95% CI 0.2-2.1), anxiety (RR=1.17; 95% CI 0.5-2.7), social anxiety (RR=1.13; 95% CI 0.4-2.7), academic distress (RR=1.51; 95% CI 0.6-3.5), eating disorder (RR=1.15, 95% CI=0.4-2.8), hostility (RR=1.26; 95% CI 0.3-3.6), family distress (RR=1.23; 95% CI 0.5-2.9), and substane use (RR=2.70, 95% CI 0.8-7.2).
Conclusion: Injured athletes had a greater overall burden of mental health issues, but most individual mental health conditions did not predict injury risk. Individual mental health conditions may not predict injury risk in collegiate athletes. These findings highlight the importance of identifying substance use and increased number of mental health concerns in athletes for injury prevention while underscoring the complex relationship between mental health and athletic performance.
Drivers of Improved Home Care Quality at Home Care Cooperatives
Authors: Geoffrey Gusoff MD MBA MS (1), Miguel Cuevas BS (2), Catherine Sarkisian MD MSPH (2), Madeline Sterling MD MPH MS (3), Ariel Avgar PhD (4), Gery Ryan PhD (5)
Affiliations: (1) Department of Family Medicine at UCLA; (2) Division of General Internal Medicine and Health Services Research at UCLA; (3) Department of Medicine at Weill Cornell; (4) School of Industrial and Labor Relations at Cornell University; (5) Department of Health Systems Science at Kaiser Permanente Bernard J. Tyson School of Medicine
Introduction: The quality of care provided by home care workers (HCWs), who serve as essential caregivers for millions of Americans, is often compromised by practices, systems, and policies that marginalize this workforce. Home care cooperatives—agencies co-owned and managed by HCWs—offer a promising approach to addressing this marginalization and enhancing care quality. However, the specific mechanisms through which the cooperative model may directly contribute to higher quality care remain unclear.
Methods: From November 2023 to June 2024, we conducted 32 semi-structured interviews with HCWs and other staff members at five home care cooperatives to explore the factors that participants believe drive improved care quality within these organizations. Interviews were recorded, transcribed, and then analyzed and coded in Dedoose using a thematic analysis approach.
Results: Respondents identified four key factors contributing to better care quality at cooperatives: greaterHCW involvement in care decisions; heightened motivation from co-ownership; a focus on hiring high-performing, mission-driven HCWs; and access to high-quality, practical training. Respondents also described particular practices and structures at the cooperative that seemed to promote each factor.
Conclusion: Cooperatives' relatively high levels of HCW care input, co-ownership motivation, caregiver selection, and capacity-building opportunities may represent important pathways for providing higher-quality home care services. Participants' responses suggest concrete practices, structures, and policies that can potentially improve care quality across the home care sector by strengthening these pathways at both cooperative and traditional home care agencies.
Quality Improvement Project Proposal: Instituting a Workflow for Starting Patients on HIV Pre-Exposure Prophylaxis (PrEP) in a Primary Care Medical Resident Clinic
Authors: Heather Wynne M.D., Hiwote Sharwargga M.D., Walter Anazonwu M.D., Mischelle Nelson M.D., Cameron Wilkinson M.D.
Affiliations: Charles R. Drew Family Medicine; Martin Luther King Jr Outpatient Center/ACN
Introduction: Each year, around 6,800 individuals in Los Angeles County unknowingly live with HIV, contributing to new transmissions amidst a syndemic of stigma and structural inequities. HIV Pre-Exposure Prophylaxis (PrEP) reduces infection risk by 99%, yet initiation remains suboptimal in primary care due to limited time with patients and low provider awareness. This quality improvement project aimed to implement a standardized PrEP initiation protocol in a primary care medical resident clinic to increase uptake and reduce HIV transmission.
Methods: We developed a workflow integrating EHR dot phrases for screening/initiation, a PrEP navigator for patient and resident support, and dedicated staff training. High-risk criteria included recent STIs, inconsistent condom use but CDC guidelines recommends PrEP for anyone interested. The protocol features same-day rapid HIV testing, 3-site STI swabs, and templated counseling. Pre-implementation data (Jan–June 2024) revealed 0 new PrEP prescriptions in our clinic, highlighting baseline gaps. Post-implementation data (August 2024–March 2025) is currently being evaluated and will be available at the time of conference presentation.
Results: Pre-implementation data (Jan–June 2024) showed 0 new PrEP initiation prescriptions for all patients seen in our clinic. Chart reviews confirmed fragmented sexual health documentation on nursing intake and no standardized screening tools for residents other than a 1 time HIV screen. Given that patients routinely present to Family Medicine clinic with STI concerns but previously were not consistently being offered PrEP or PEP. These findings underscored systemic barriers, including workflow gaps and knowledge deficits. Post-implementation evaluation (August 2024–Mar 2025) is ongoing, with results analyzing PrEP initiation rates, adherence, and workflow efficiency. Results available by time of conference.
Conclusion: Pre-implementation data confirmed critical gaps in PrEP initiation, including absent workflows and low provider/patient awareness in the setting of a busy resident clinic. This project addresses these barriers through a structured protocol integrating screening, EHR tools, and navigator support, in the hopes of easing this process into resident clinic in a way that is manageable and sustainable to decrease new HIV diagnoses in our community. Post-implementation data, available at conference presentation, will evaluate the protocol’s impact on uptake and adherence, offering insights for scaling
Evaluating the Impact of Cold Water Immersion on Recovery and Performance in Division I Athletes
Authors: Jeremy Swisher, MD, Joshua Goldman, MD, MBA, Brian Donohoe, MD, Jeremy Vail, PT, SCS, OCS, Jeonguen Kim, MBI, Calvin Duffaut, MD, Nicolas Hatamiya, DO, Nelson Boland, MD
Affiliations: UCLA Division of Sports Medicine
Introduction: Cold water immersion (CWI) is a popular recovery method among athletes, yet its physiological effects and performance benefits remain debated. While some studies support reductions in muscle soreness and improved perceived recovery, objective data in elite athletic populations remains limited. With the growing use of wearable technology, researchers can now assess recovery interventions in real time and with greater precision. This study combines biometric data and athlete-reported outcomes to evaluate the effects of CWI on recovery and performance in NCAA Division I athletes during a high-intensity training cycle.
Methods: Thirty-seven NCAA Division I athletes participated in a four-week training cycle while wearing WHOOP devices to monitor HRV, RHR, and sleep. During the two-week intervention, athletes completed ten-minute cold water immersions at 53°F within one hour of training, five days per week. Daily REDCap surveys assessed subjective recovery, sleep quality, and muscle soreness. Weekly countermovement jump tests measured performance. Mediational multilevel models were used to analyze outcomes in the full sample and in a defined subgroup of responders who showed HRV increases following CWI.
Results: In the full sample, CWI did not significantly impact HRV, RHR, sleep duration, or performance metrics. However, it was associated with a small but significant reduction in muscle soreness (p = 0.013). Subgroup analysis of responders, athletes who showed HRV increases post-CWI, revealed significant improvements in HRV (p = 0.017), RHR (p = 0.016), and perceived recovery (p = 0.008). CWI also directly improved HRV independent of subjective recovery (p = 0.004). Muscle soreness reduction in responders was over twice that of the full sample (p = 0.0004).
Conclusion: While CWI did not demonstrate significant improvements in objective recovery or performance metrics across the full sample of NCAA Division I athletes, subgroup analysis revealed potential benefits for a subset of responders. In this group, CWI enhanced subjective recovery and HRV and reduced RHR, suggesting a targeted role for CWI in individualized recovery strategies.
Tell Me More About Your Low Back Pain: A Quality Improvement Initiative
Authors: Kayvon Seyed Dehghanian, MD, Monique Gonzalez-Johnson, MD, Arash Karimi Afshar, DO, Jose Rodrigo Gonzalez-Correa, MD
Affiliations: Mission Community Hospital Family Medicine Residency Program
Introduction: Low back pain (LBP) is the leading cause of disability worldwide. (1) LBP is typically classified based on duration. (2) Treatment options include pharmacologic, non-pharmacologic, and watchful waiting. (3, 4) Advancing to treatment without thorough evaluation and documentation of LBP can result in misdiagnosis and ineffective management. (5, 6) This quality improvement project aimed to increase the percentage of patient visits that included documented standardized pain assessments and appropriate follow-up plans for LBP.
Methods: We conducted a review of two months' worth of visits at our continuity clinic, Santo Nino, focusing on adult patients diagnosed with LBP, identified using the ICD code M54.5. We analyzed 27 relevant visits to evaluate the documentation of LBP onset and severity, specifically using the Visual Analog Scale (VAS), as well as the adequacy of follow-up plans. Adequate follow-up was defined as medication management, imaging, referrals, or watchful waiting, complemented by clear return-to-clinic (RTC) instructions. To improve documentation of pain assessments and follow-up plans, we introduced visual reminders in the form of posters and telephonic group messages. A follow-up review was conducted two months after implementation to assess our progress.
Results: Initially, only 33.3% of the notes documented LBP severity using the VAS, whereas 70.3% noted the onset of LBP clearly, and 74% included adequate follow-up plans. Overall, just 22.2% of the reviewed notes contained documentation of LBP severity with the VAS, a clear onset time, and appropriate follow-up plans. After two months of implementing visual and telephonic reminders, we reviewed 33 relevant visits. The results showed that 36.3% of the notes documented LBP severity with the VAS, 57.5% indicated the pain's onset clearly, and 87.8% provided adequate follow-up plans. Overall, 33.3% of the notes documented LBP onset, severity, and care plans adequately. Please refer to Table 1 for the complete results of the study.
Conclusion: When face-to-face handoffs are not feasible, physicians rely on prior visit notes to tailor care plans. Therefore, precise documentation is essential for enhancing patient care. Our initiative involved simple visual cues and reminders, which resulted in a 50% relative increase in the documentation of LBP severity using the VAS, clear onset times, and proper follow-up plans. Post-intervention, 87.8% of the notes included adequate follow-up plans. However, only 36.3% of the documentation stated clear LBP severity. Future efforts should focus on improving this aspect of documentation.
-
Chronic Diarrhea: A Case Report of Eosinophilic Gastroenteritis
Authors: Matthew Quan MD, Weiwei Liu MD, Lucia Vulcan MD MPH, Bernadette Pendergraph MD, Gloria Sanchez MD FASAM
Affiliations: Department of Family Medicine at Harbor-UCLA Medical Center
Introduction: Eosinophilic gastroenteritis (EGE) is a rare disorder with a highly variable presentation and is more commonly seen in children compared to adults. We present the case of a 49-year-old male who presented with approximately 3 months of profuse watery diarrhea, 40 lb. weight loss, and significant evidence of protein wasting, leading to a diagnosis of EGE. This case sheds light on a rare diagnosis and demonstrates the importance of identifying when an expedited work up including colonoscopy is necessary.
Methods: 49-year-old-male with PMH of heart failure, HTN, DM2, CKD, and CAD was admitted with dehydration related to 10-15 watery stools per day, nocturnal diarrhea, right lower quadrant and right flank tenderness with a CT showing enterocolitis of the small bowel and ascending colon. His infectious disease work up was negative with no leukocytosis, negative stool studies (stool culture, C. difficile, ova and parasite). His inflammatory work up was positive with elevated ESR, CRP, fecal calprotectin but normal studies for celiac disease. Labs showed nutritional deficiencies of iron, vitamin K, vitamin A, and total protein. A colonoscopy and capsule endoscopy showed extensive bleeding ulcers in the jejunum, ileum, and ascending colon with biopsy showing eosinophilic gastrointestinal disease. To control symptoms, he was started on anti-diarrheal agents, and an elimination diet that removed the most frequent food allergens: milk, eggs, soy, wheat, nuts, and fish. Repeat ERCP showed improvement in the ulcerations, but further biopsies were obtained of the stomach and proximal small intestine.
Discussion: This case demonstrates a rare cause of severe diarrhea that led to malnutrition and prolonged admission. Given the CT results showing both small and large bowel involvement, Crohn’s disease was initially suspected. We did not consider eosinophilic gastrointestinal disease until the pathology was reviewed. This condition takes time to respond to intravenous corticosteroids and elimination diets are key to improving symptoms. As busy ambulatory family medicine physicians, it is important to expedite serology and/or diagnostic studies when patients endorse diarrhea lasting longer than 2 weeks. Future studies should explore how inflammatory gastrointestinal disorders can affect pain, quality of life, and functional status.
New Aquagenic Urticaria “Water Allergy” in 14 Year Old Male With No Past Medical History
Authors: Michael Jaso, DO, Eric Gama, MD
Affiliations: Department of Family Medicine at Dignity Health - Northridge Medical Center
Introduction: 14 year old male with no past medical history having new onset urticaria and pruritus with water contact to skin. Aquagenic Urticaria (AU) “water allergy” is a rare condition characterized by the development of urticaria (hives) upon contact with water. It is an unusual form of physical urticaria, and the exact etiology remains poorly understood with a few mechanisms postulated. Because of the unknown etiology there are inconsistent and mixed results with current interventions and further research is needed for this potentially life-altering condition.
Methods: 14-year-old male without past medical history with new onset AU “water allergy” starting in June 2024. Initially had itchy red blotches on his bilateral thighs shortly after showering, which self-resolved within 20-30 minutes. No recent changes or additions to hygiene, diet or environment within 2 months prior to onset of symptoms. Subsequent water contact demonstrated urticaria localized to his neck, chest, and upper back only. Symptoms also occur from several different water sources including tap water and bottled water (multiple brands). Asymptomatic with changes in temperature (hot or cold) and with drinking water. Urticaria continues to self-resolve within 30 minutes after water contact stops and no other symptoms occur. Symptom management with 2nd generation H1 antihistamines including trial of Loratadine 10mg daily, Fexofenadine 180mg daily, and Diphenhydramine 25mg 30-45 minutes before water contact. Treatment has decreased urticaria and pruritus but did not fully prevent symptoms. Currently being evaluated by an Allergist for possible further testing and interventions.
Discussion: This case highlights the rare presentation of AU along with bringing awareness of uncommon allergies. Although the etiology remains unclear, treatment with antihistamines appears to provide some symptomatic relief, albeit historically not always complete resolution. This case underscores the importance of considering AU in patients presenting with pruritic skin reactions to water or water and emphasizes the need for further education, training and research into effective recognition of condition and management strategies.
Unmasking Catastrophic Antiphospholipid Syndrome: A Rapidly Progressive Case of Multiorgan Thrombosis
Authors: Arghavan Jafarijozani MD; Sabrina Afroz MD; Monique Gonzalez-Johnson MD
Affiliations: Mission Community Hospital
Introduction: Catastrophic Antiphospholipid Syndrome (CAPS) is a severe, rapidly progressing form of antiphospholipid syndrome, leading to multiorgan thrombosis, thrombocytopenia, and hemolytic anemia. It involves antiphospholipid, lupus anticoagulant, and anticardiolipin antibodies. Treatment includes anticoagulation, steroids, plasma exchange, cyclophosphamide, and immunoglobulin. With a 50% mortality rate, early diagnosis is critical. This case report presents a 41-year-old female with multiorgan thrombotic events
Methods: A 41-year-old Filipino female (G1P1) with no significant medical or obstetric history presented to the MCH ER with a 3-day history of fatigue, dyspnea, orthopnea, oliguria, multiple ecchymoses, and a hypertensive crisis. Labs showed severe acute renal failure, hemolytic anemia, thrombocytopenia, and elevated troponin I without EKG changes, requiring ICU admission. Initial management included blood transfusion, BP control with nicardipine infusion, aspirin, and hemodialysis. Imaging studies revealed moderate Mitral and aortic regurgitation on TTECHO, and occlusive thrombus in the right jugular vein on Doppler US, while further tests showed positive ANA and lupus anticoagulant antibodies, ruling out TTP. Suspecting an SLE flare-up, pulse steroid therapy was initiated, but the patient suffered an acute thalamic infarct on day 3. Due to resource limitations, she was transferred to a higher-level facility for further care
Discussion: This case highlights the diagnostic complexity of Catastrophic Antiphospholipid Syndrome (CAPS), marked by multi-system thrombotic events requiring urgent intervention. The patient's acute presentation—severe microangiopathic hemolytic anemia, hypertensive emergency, acute kidney failure, DVT, and thalamic infarct—strongly suggests CAPS, especially with positive antiphospholipid antibodies and thrombocytopenia. Given its high mortality, early recognition and aggressive treatment are critical for improving outcomes.
Etiology of Epistaxis in the Primary Care Clinic: Beyond dry nose and digital manipulation. A case of newly diagnosed Hemophilia A in a 14-year-old male
Authors: Natalia Henriquez, MD, Andrea Ayala, MD
Affiliations: Mission Community Hospital Department of Family Medicine
Introduction: Epistaxis is a very frequent health complain. Approximately 60% of people in the United States will experience nosebleeds at some point in their life. Its peak frequency occurs in children less than 10 years old and adults between 70 and 79 years old. In children, it’s usually self-limited and associated to digital trauma, crusting from nasal inflammation, or nasal foreign bodies. In this case, however, what initially appeared as benign epistaxis, finally required further workup and led to the diagnosis of an uncommon hematologic disease.
Methods: We present a case of a 14-year-old male with no significant medical history, brought to our primary care clinic for a Well child exam. Patient’s mother voiced concern about his frequent nosebleeds. She reported he has had nosebleeds since childhood, but they have become more frequent, happening almost daily. Denied nasal congestion or "nose picking". Also denied easy bruising, hematuria, or hemarthrosis. He did report bleeding longer than normal with dental procedures. Mom noted that her uncle, her brother and one of her nephews had problems with increased bleeding. She recalled that her uncle was once hospitalized for a severe hemorrhage. Hematologic studies where ordered, beginning by a complete blood count, Prothrombin time and Partial thromboplastin time (PT/PTT). Hemoglobin, platelet count and PT where normal, but PTT was prolonged at 57.8. Further testing was done, measuring Von Willebrand factor (vWF) antigen and Factor VIII. VWF was normal, but Factor VII was 8 (reference interval 69-237%). He was therefore referred to Hematology, and was diagnosed with Hemophilia A.
Discussion: Hemophilia A is a rare X-linked recessive disease, affecting 12 per 100,000 males in the United States. It is caused by a mutation in the genes that code for clotting factor VIII. In the case presented, the patient only reported mild bleeding, which would normally lead us to a conservative diagnostic approach. However, a family history of three males of different generations with severe bleeding issues, was the key factor in suspecting a hereditary cause. Our duty as primary care physicians is therefore to stay vigilant. We need to assure we don’t miss significant diagnosis, while continuing to use resources wisely. After diagnosis, we have a role in notifying the school about the disease, ordering contact sports restrictions, and requesting permanent access to emergency medications.
CNS Under Siege: Meningoencephalitis as a Manifestation of Behçet’s Disease
Authors: Sheila Toro, MD, MSc; Jacqueline Garcia, MS IV; Stephanie Garcia, MD; Yvette Singh, MD; Verna Marquez, MD
Affiliations: Clinica Sierra Vista
Introduction: Behçet syndrome is a rare, systemic vasculitis characterized by recurrent oral and genital ulcers, ocular involvement, and multisystem complications. Neurological manifestations, known as Neuro-Behçet syndrome (NBS), occur in 5–10% of cases and can mimic central nervous system (CNS) vasculitis, demyelinating diseases, or ischemic stroke. This case report describes a young male presenting with neurological symptoms, oral ulcers, and meningo-vasculitis, raising suspicion for NBS.
Methods: Diagnostic procedures included lumbar puncture, which revealed elevated CSF white blood cells and protein, and MRI brain imaging showing signs of subacute ischemia or vasculitis. Extensive infectious and autoimmune panels were largely negative, except for positive EBV IgG. The patient underwent laryngoscopy and lymph node biopsy, with results pending at discharge. A multidisciplinary team, including neurology, rheumatology, and infectious disease specialists, concluded that the symptoms were consistent with CNS manifestations of Behcet syndrome presenting as meningo-vasculitis. The patient was treated with high-dose oral steroids and discharged with follow-up plans for outpatient care and further diagnostic evaluation.
Discussion: MRI findings of subacute ischemia and inflammatory CSF indicated a CNS inflammatory process. Laboratory workup ruled out infectious and most autoimmune causes, with EBV IgG positivity of uncertain significance. Despite the negative pathergy test and incomplete diagnostic criteria, Behçet syndrome remained a leading consideration due to the neurological symptoms and oral ulcers. The patient showed improvement in right-sided weakness following corticosteroid therapy. This case emphasizes the need for clinical vigilance in recognizing Neuro-Behçet syndrome, even in the absence of definitive diagnostic criteria. Early consideration and prompt immunosuppressive therapy can lead to favorable outcomes, highlighting the importance of a multidisciplinary approach in managing complex CNS inflammatory conditions.
Silent Invader: A Rare Case of S. Pyogenes Pneumonia in an Asymptomatic Host
Authors: Allison Siu, DO
Affiliations: UCR/ RUHS Family Medicine Residency
Introduction: Streptococcus pyogenes pneumonia (SPP) typically presents with symptoms of sore throat, fever, and cough. Atypical or asymptomatic presentation of patients with SPP is uncommon. Early detection of SPP is crucial due to its historically high mortality rate and requirement for intricate critical care management strategies. This case report presents a 47- year- old male with complaints of worsening chronic shortness, without significant signs of acute infection, who was found to have a severe left sided plueral effusions with positive cultures for strep pyogenes.
Methods: A 47-year-old male presents with a complaint of orthopnea for 1 month. His primary doctor attributed his orthopnea to worsening renal disease. At a subsequent clinic visit she noted diminished left-sided breath sounds, ordered a chest x-ray, and consequently sent the patient to the ED for further management of left-sided pleural effusion. His medical history includes ESRD on dialysis and diabetes. He is a non-smoker and denies heavy alcohol use.
On presentation to the ED, the patient was hemodynamically stable on room air. Labs indicated normocytic anemia but was otherwise normal. Pleural studies were consistent with parapneumonic exudative effusion with SAAG 0.4. Patient was started on ceftriaxone and doxycycline. Bronchioloalveolar lavage revealed predominant Strep and Neisseria flavescen (oral colonizer). VAT surgery was notable for empyema with surgical cultures positive for a colony of Streptococcus pyogenes. Upon obtaining these cultures, metronidazole was added to the current antibiotic regimen. The patient was discharged with 6 weeks of antibiotics and supplemental oxygen.
Discussion: SPP typically presents with acute onset upper respiratory symptoms of fever, chills, and cough, however, this case highlights that patients do not always fit into the classic presentation for this rare type of pneumonia. Although previously known to be a rare cause of pneumonia, with only 16 adult cases reported from 1986-2016, this case report demonstrates that SPP is becoming more prominent, with at least 7 new adult cases of SPP reported in the last 8 years.
Only a minority of patients with pneumonia will require intervention for a complicated pleural effusion or empyema. SPP makes up about 30-40% of documented cases of explosive pleuritis, a pleural effusion that significantly increases in size in less than 24 hours and is associated with rapid clinical deterioration.
Isolated Medial Elbow Dislocation without Concomitant Fracture in an Adult Snowboarder
Authors: Betty Hom MD (1), Kirin Escher MD (2), Austin Meng MD (3)
Affiliations: (1) Sports Medicine Fellowship, Kaiser Permanente Los Angeles; (2) Sports Medicine Fellowship, Long Beach Memorial Care; (3) Department of Emergency Medicine, Renown Regional Medical Center
Introduction: Posterior and posterolateral elbow dislocations are most common, while medial or lateral dislocations are rare and often require reduction under general anesthesia. Most cases involve periarticular fractures, making purely soft tissue/ligamentous “simple” dislocations less common. This case reviews an adult male with an isolated, simple medial dislocation from a FOOSH injury. With limited literature on reduction techniques for these cases, we outline a successful closed reduction performed in an urgent care setting without sedation.
Methods: 38-year-old male was brought to Urgent Care by ski patrol for left elbow pain after falling on his outstretched arm while snowboarding. Exam revealed loss of normal olecranon contour, valgus deformity with a medial protrusion, and tenderness at the olecranon fossa. ROM was limited due to pain. RUE remained neurovascularly intact.
AP radiographs showed the radial head articulating with the trochlea and the proximal ulna displaced medially. The radial head appeared normal on lateral view, while the ulna overlapped the capitellum. He was diagnosed with a medial elbow dislocation and received intra-articular bupivacaine blocks and IM fentanyl to prepare for a closed reduction.
Axial traction was applied to his flexed, supinated forearm, while direct pressure was placed onto his medial elbow. This was repeated, followed with hyperflexion. On final attempt, the elbow was extended and forearm maximally pronated, with medial pressure applied, until it yielded a distinct "clunk". Successful reduction was confirmed on imaging before immobilizing the elbow with a long-arm posterior splint.
Discussion: Even after successful reduction, patients should follow up with an orthopedist due to the higher rates of recurrent instability and ulnar neuropathy seen in medial elbow dislocations compared with other displacement patterns. Ligamentous injuries in pure medial dislocations typically involve the LCL and forearm extensor tendons. Treatment is usually non-operative, involving closed reduction (often with sedation), short-term immobilization, and a supervised rehab program emphasizing early range of motion. Surgical management is considered for recurrent instability or neurovascular compromise.
The Price of Paradise
Authors: Bijan Origel, D.O., Rabiah Fresco, MD, Crystal Estrada MD, Jeff Ijadi, MD, Jesse Cheung, MD, Jay Shah, D.O.
Affiliations: Pomona Valley Hospital Medical Center
Introduction: Surfer’s myelopathy is a rare non-traumatic spinal cord injury commonly affecting first time surfers. There are fewer than 100 reported cases of surfer’s myelopathy with most of the reported cases occurring in high surfing communities like Hawaii. As surfing continues to grow in popularity more people will be impacted. As was this case of a 16 year old teenager developing surfers myelopathy after surfing for the very first time. The risks that come with surfing aren’t commonly discussed in the public. Therefore, further awareness and education is needed in order to prevent future cases.
Methods: 16 year old male with no significant PMH presented to ED for bilateral lower extremity numbness and weakness. Patient was on vacation in Maui, where he took a one hour surfing lesson for the first time. Patient denied any wipeouts or traumas. After completing his lesson, he was able to walk back to the hotel without difficulty. Patient noted 1 hour later, he started experiencing some limping, leg weakness, and lower back pain that then progressed to the inability to walk, void, or stool. After 24 hours of no improvement, patient came into the ED. In the hospital, physical exam was notable for a distended abdomen, and bilateral lower extremity flaccid paralysis. Labs including CBC and BMP were all within normal limits. Diagnostics were notable for a MRI thoracic/Lumbar spine without IV contrast for abnormal T2 hyperintense signal in the central spinal cord extending from T7 to conus with mild expansion. Patient was treated with a urinary catheter, IV fluids, aspirin and physical therapy. Upon discharge, patient was unable to walk or void and was sent to inpatient rehab facility.
Discussion: Surfer’s Myelopathy is a rare non-traumatic spinal cord injury associated with first time surfers. The most common symptoms include back pain, sensory loss, paraplegia, lower extremity weakness, and urinary retention. The exact cause of surfer’s myelopathy is still unknown. However, it is commonly believed that prolonged hyperextension leads to vascular damage in the distal portion of spinal cord. It is theorized that first time surfers are more likely to be in this prolonged hyperextended state than experienced surfers. As surfing has become increasingly popular each year and with no standardized treatment, it is therefore important to educate preventative measures in avoiding SM. This includes education on proper maneuvering techniques to prevent prolonged hyperextension.
Gas Below the Belt: A Case of a Cryptic Duodenal Perforation
Authors: Haig Karsian DO, Divya Chopra MD, Jan M. Schilling MD, Sabrina Wedee DO, Belonwu Okafor MD, Andrew Kim MD, Daniel Yousefzadeh MD, Amit Grover MD, Liliana Bustamante MD
Affiliations: Department of Family Medicine at Mission Community Hospital
Introduction: Subcutaneous emphysema (SE) is the presence of air within soft tissues, with an incidence of 0.43%–2.34% [1,2]. Lower extremity SE is rare & typically results from trauma/infections by gas-producing organisms [3-7]. However, there are rare cases of air from a perforated hollow viscus transversing fascial planes to distant regions as well [3-9]. Usually, these types of perforations are from colonic sources, with only a few cases that have been reported [4,6,7,10,11]. Small intestinal perforations, as in our case, are extraordinarily rare [5]. Moreover, duodenal perforation’s mortality rate ranges from 8% to 25% [12].
Methods: We report a 62-year-old male with HTN, HLD, HCV, & gout who presented with worsening chronic bilateral knee pain ×5 days (L > R), described as achy & 10/10, worsened by walking & relieved by rest/ibuprofen. He denied trauma, fever, malaise, anorexia, abdominal pain, N/V. Exam showed L knee swelling, crepitus, warmth, & decreased range of motion, without signs of cellulitis or external infection. Abdomen was soft with mild fullness, non-tender. Vitals: tachycardia, leukocytosis. CT L knee showed soft tissue gas without myonecrosis, concerning for gas gangrene. Further CT C/A/P revealed duodenal perforation, pneumoperitoneum, & a 13.2 cm RUQ abscess. The patient underwent emergent laparotomy & IR drainage but ultimately succumbed to complications.
Discussion: Lower extremity SE due to duodenal perforation is exceedingly rare [5] & can mimic gas gangrene, leading to potential misdiagnosis. Retroperitoneal air dissection without abdominal symptoms presents a diagnostic challenge. Mortality can reach 50%, particularly with abscess formation [13]. This case emphasizes the need for early recognition of unexplained soft tissue gas & a broad differential diagnosis. Clinicians should consider intra-abdominal sources in patients with atypical SE to prevent delays in life-saving treatment.
Lactobacillus infective endocarditis following colonoscopy
Authors: Cody Webb, MD
Affiliations: Kaiser Permanente Los Angeles, Family Medicine Residency
Introduction: Lactobacillus is a gram-positive rod whose presence in the human gut microbiome is supportive of a healthy intestinal barrier. It is commonly found as a probiotic supplement and generally considered as safe, however there are a few documented cases of infection such as bacteremia, infective endocarditis, urinary tract infection, pneumonia, and abscess. This report will describe a case of Lactobacillus infective endocarditis following a colonoscopy. This rare case report seeks to bring attention to lactobacillus as a rare cause endocarditis and colonoscopy as a predisposing risk factor.
Methods: An 80-year-old male with history of Parkinson’s, mild-moderate mitral regurgitation presented to the ED for an accidental overdose on Sinemet; he noted lightheadedness and diarrhea. After a short monitoring period, the patient’s symptoms resolved. Blood cultures were drawn due to fluid-responsive hypotension and resulted positive for Lactobacillus rhamnosus, confirmed with repeat culture. The patient was admitted for evaluation of a source and started on penicillin G and synergistic gentamycin. Urinalysis and CT abdomen were unremarkable. A TEE showed a 2mm x 2mm, mobile, echogenic structure that was consistent with a small vegetation.
The patient completed six weeks of penicillin G and two weeks of gentamycin. One-week post-treatment, he experienced altered mental status; MRI brain revealed septic emboli, though TTE showed no vegetations and cultures were negative. He returned to baseline function without deficits. Shortly thereafter, he developed Clostridium difficile infection, was treated with vancomycin, and started on Lactobacillus rhamnosus probiotics.
Discussion: This case of lactobacillus endocarditis with subsequent septic emboli represents one of a few documented cases following colonoscopy. Previous narrative review found that 17.3% of patients with lactobacillus endocarditis were taking probiotics. While this patient had no prior probiotic exposure, their subsequent probiotic use raises questions about safety in patients with risk factors for infection. Further research is needed to assess the risks of probiotics pre-colonoscopy and their use in patients with a history of Lactobacillus endocarditis.
Lectern Session 1 (1:40 – 2:25PM)
-
Authors: Maria Malave Gomez, MD (1); Yaritza Santos, MD (2); Danish Khalid, MD (2); Hector Arreaza, MD (1)
Affiliations: (1) Clinica Sierra Vista; (2) Kern Medical Center
Introduction: Obesity and mood disorders, particularly depression and anxiety, are major global health challenges that significantly impact quality of life and burden healthcare systems. Despite their high prevalence, the complex relationship between these conditions remains underexplored. This study examines the bidirectional association between obesity and mood disorders, focusing on shared pathways and causal links. Findings aim to inform integrated prevention addressing both physical and mental health to improve outcomes for individuals affecting by these intertwined conditions.
Methods: This study explores the correlation between obesity and depression within the patient population of Clinica Sierra Vista (CSV), a rural healthcare institution in California's Central Valley serving predominantly low-income and underserved communities. Utilizing a retrospective design, data from 42,646 patients aged 18-99 were analyzed through chart reviews of BMI and PHQ-9 scores recorded in the EPIC systems from January 1st, 2022 to January 1st, 2024. Inclusion criteria included BMI ≥30, PHQ-9 ≥5 and GAD-7 ≥5, while patients with BMI <30 or PHQ-9 or GAD-7 scores ≤4 were used as a control group. Exclusion criteria included any patients under the age of 18.
Results: We analyzed data from 42,646 patients (67% female, 33% male, 3 excluded due to missing gender). The female-to-male ratio was 2:1. Average age was 46 years old, mean BMI was 35.75. A significant positive correlation was found between BMI and GAD-7, stronger in females than males. Logistic regression showed BMI significantly predictive anxiety, with obese patients having 1.10 times higher odds of anxiety. For every 5-unit, BMI increase odds of anxiety rose by 10%. Using PHQ-9 and BMI as continuous variables, there was also a significant positive correlation, stronger in females than males with an odds ratio of 1.14. Meaning for every 5-unit BMI increase, odds of depression rose by 14%. Results emphasized the interplay between BMI, anxiety and depression, especially in females.
Conclusion: Our research highlights a significant link between BMI, anxiety and depression, emphasizing BMI's role in mental health. Limitations include potential confounders such as gender misrepresentation, cultural norms, socioeconomic status, healthcare access and reliance on self-reported data. Future research should explore the pathophysiology and relationship between obesity and depression; focusing on obesity-centered approaches. Future research will include data on PHQ-9 after semaglutide (vs others), potentially proving that weight loss improves mental health outcomes.
-
Authors: Alexandra Rabotin, MD and Jose R. Gonzalez-Correa, MD
Affiliations: Mission Community Hospital Family Medicine Residency Program, Panorama City, CA
Introduction: The rise of ambient artificial intelligence (AI) scribing systems in healthcare raises concerns about the inclusivity of the generated content. It is uncertain whether these systems inherently follow best practices or if they require explicit prompts to support inclusivity. We aimed to assess the impact of a customized prompt, based on the Inclusive Language and Context Style Guidelines (American Medical Informatics Association, 2023), on the inclusivity of AI-generated clinical notes.
Methods: The ambient Doximity AI-scribe (GPT-4, beta version) was used by a single second-year family medicine resident in a continuity clinic from November 5, 2025, to January 6, 2026. Verbal informed consent was obtained from each patient and/or guardian. A customized prompt was added: “Please ensure adherence to Inclusive Language and Context Style Guidelines,” with a direct link to the guidelines. Notes were reviewed for language differences by the resident and confirmed by a supervising attending. Differences were categorized into seven groups. The patient’s age, assigned sex at birth, and interpreter use during the encounter were also recorded. A one-tailed binomial test was used to determine whether the proportion of inclusive changes exceeded chance (p < 0.05 considered significant).
Results: We analyzed 39 AI-scribed notes from 41 patients (44% assigned male at birth; age range 0–87 years; median age 27 years [IQR 11–55]). An interpreter was used in 51% of encounters (86% in Spanish). A total of 65 differences related to inclusive language were identified between prompted and non-prompted notes. The most frequent category was non-stigmatizing language (30.8%), followed by gender neutrality (20.0%), supportive tone (13.8%), neutral clinical framing (9.2%), shared decision-making (9.2%), age neutrality (7.7%), and other (9.2%). The majority of changes (86.2%) reflected improved inclusivity (binomial test, p < 0.01).
Conclusion: Explicit prompts may improve adherence to inclusive language guidelines in AI-scribed clinical notes. Such prompts have the potential to enhance documentation quality by reducing stigmatizing language and promoting gender neutrality, a supportive tone, and shared decision-making. Nonetheless, occasional shifts toward less inclusive language highlight the need for continued evaluation, refinement, and prompt optimization.
-
Authors: Cecilia Cusimano Murillo MD; Irene Velarde DO, Tung Chu DO, Daniel Blocker PhD, Douglas Chiriboga MD, Jesse Cheung MD, Maria Christina Tolentino DO
Affiliations: Pomona Valley Hospital and Medical Center
Introduction: A step to increase the number of underrepresented minority (URM) physicians and providers is to spark interest and provide role models while students are in high school and college. This project tested an ongoing curriculum to increase exposure and promote interest in a career in healthcare for URM students living in an underserved area by partnering with Bright Prospect, a foundation which provides counseling and support for students through high school and college years. We will share resources, methodology, and techniques used to develop, implement, evaluate, and improve the curriculum in an iterative process spanning over 7 years.
Methods: Over the span of 7 years, family medicine residents collaborated with a community organization to host interactive workshops for high school students and college students. These workshops focused on community education and empowerment with common medical problems as well as career development. Results were measured by analyzing pre- and post-curriculum surveys which assessed the attitudes and beliefs regarding pursuing any career in the healthcare field and included key social-emotional competencies.
Results: From 2018-2024, 130 students completed a pre-survey and 67 completed a final post-survey. On 5-point Likert scales (1=Strongly Disagree; 5=Strongly Agree), the most significant increase was in: “I am confident in my understanding of the pathway of getting into medical school,” with a pre-mean of 3.51 and post-mean of 4.21 (Hedges G of 0.76, indicating a moderate to large effect size). Student pre and post answers were also analyzed using a student’s Cohen’s D test. After completing the workshops, there was a moderate effect on students’ confidence in their understanding of the pathway to getting into medical school with a Cohen’s D score of 0.61. Students reported improvements in other fields, although the effect size of these was considered small. This year's data is pending.
Conclusion: Our project demonstrates a successful, longitudinal collaboration between a residency and a community organization. Pre and post surveys indicated moderate improvement in student confidence in the path to become a physician. Future directions include assessing interests in other healthcare careers, additional workshops, improving outreach for college students, reaching out to more grade schools in the community. In addition, the final consensus expressed interest in non physician roles and future curriculum can address these interests.
-
Authors: Ajinkya Mawley, DO; Omar Abdalla, DO; Shane Rayos Del Sol, MD; Susan Li, DO; Esther Zarecki, MD; Faheem Jukaku, MD; Raymond Kramer, MD
Affiliations: Riverside University Health System/ UC Riverside
Introduction: More than 1 million people have died from drug overdose since 1999. Overdose from opioids makes up 76% of all drug overdose deaths. Increasing the availability of treatment has led to estimates of a 13-27% decrease in overdose fatalities. Unfortunately, the majority of patients do not receive OUD treatment due to the low adoption rate of MAT from providers. In this study, we aim to quantify the impact of MAT for our patients with OUD in a single clinic in Riverside County. We hypothesize that patients who seek and regularly receive MAT due to OUD have reduced ED visits when compared to patients with OUD that do not receive MAT.
Methods: This is a retrospective study looking at the effectiveness of MAT in patients diagnosed with OUD in a single clinic in Riverside County between 2019, when MAT services initiated, to 2023. We hypothesize that patients diagnosed with OUD with MAT services would have decreased ED usage. Inclusion criteria are patients who are at least age 18 with diagnosis of OUD. Those with only one MAT visit were excluded. The primary outcome is a reduction in ED visits. A Wilcoxon signed-rank test was used to compare the number of ED visits 1 year before and 1 year after MAT clinic initiation. Outliers were excluded using the interquartile range (IQR) method. A p-value < 0.05 was considered statistically significant.
Results: A total of 53 patients were analyzed, with 7 patients being classified as outliers. Therefore, 46 patients who established care at the MAT clinic prior to December 2022 and had complete ED visit data were included in the analysis. The mean number of ED visits decreased from 1.46 (SD = 1.76) before MAT to 0.35 (SD = 0.57) after MAT, yielding a mean reduction of 1.11 visits. A Wilcoxon signed-rank test showed this reduction was statistically significant (p = 0.00005). Among patients with more than 3 MAT visits (n = 32), the reduction was also significant (mean = 1.31 visits, p = 0.0003). These findings support the effectiveness of MAT in reducing ED visits.
Conclusion: OUD continues to drive high rates of ED utilization due to medical complications and lack of consistent care. Our findings add to evidence that MAT reduces acute care needs. Even in a small community setting, MAT led to meaningful ED reductions—especially for those with >3 visits, highlighting the value of continuity. The MAT clinic’s dual role as primary care may have improved access and outcomes. While promising, results are limited by small sample size and potential confounding variables. Larger studies are needed to confirm and guide implementation.
Poster Session 2 (2:25 – 3:05PM)
-
Rethinking Heat Risk: A Community-Partnered, Digitally Integrated Toolkit for Heat Illness Screening
Authors: Milan V. Carter, BS (1), Beza Mengistu, BS (1), Gladys Bello, BS (1), Gerardo Arteaga, BS (1), Ann Marie Hernandez, MD (2), Sherill Brown, MD (3)
Affiliations: (1) David Geffen School of Medicine at University of California Los Angeles, Los Angeles, CA, USA (2) Department of Family Medicine at UCLA (3) AltaMed Health Services
Introduction: Low-income and minority communities in urban heat islands can experience temperatures up to 15 degrees higher than surrounding areas. Heat-related illness (HRI) poses a significant health risk to vulnerable populations, including pregnant individuals, those with comorbidities, and social determinants of health (SDOH) challenges. Yet, fewer than 5% of clinical screening tools address environmental health. Through a community-partnered research model, we sought to integrate a heat illness screening tool incorporating SDOH factors to identify at-risk patients within the AltaMed system.
Methods: A PubMed literature review revealed limited tools addressing both heat illness and SDOH. In partnership with AltaMed, a federally qualified health center, we will conduct a mixed-methods study to assess current screening practices and develop a health illness screening toolkit. Our team includes clinicians, medical students, and academic researchers. Through iterative stakeholder meetings, we developed a 13-question survey to be distributed to 30 physicians to assess baseline screening behaviors. Findings will inform a guide tailored to the clinic’s patient population and risk factors. Physician-facing education will be delivered with pre/post-surveys analyzed via descriptive statistics. Culturally tailored, patient-facing toolkits will be co-developed with the Patient Advisory Group.
Results: We expect that while most providers will recognize the importance of heat illness, few will report actively screening for it. Anticipated barriers include time constraints, lack of tools, and uncertainty about identifying at-risk patients. Post-intervention data collection will inform physician implementation measures. Digitized patient-facing materials will be developed and reviewed by the Patient Advisory Group for accessibility and cultural relevance.
Conclusion: Community-partnered approaches can inform culturally relevant tools to screen for heat-related illness in high-risk populations. Preliminary findings suggest low screening rates and limited provider awareness, revealing a critical gap in care. Integrating SDOH into workflows and developing simple, streamlined assessment measures - such as EHR-based prompts and educational toolkits - can support early screening. Ongoing physician education and patient engagement are essential to drive implementation and promote health equity.
Survey of UCLA Health Family Medicine Physicians Reveals Gaps in LGBTQIA+ Training Regarding A-spec Identities
Authors: Maria G. Luna, BA (1), Jesse Clark, MD (1,2)
Affiliations: (1) University of California, Los Angeles, David Geffen School of Medicine, Los Angeles, United States; (2) Department of Family Medicine at UCLA
Introduction: Asexuality (ace), aromanticism (aro), and agender (agen) (“a-spec” identities, the “A” in LGBTQIA+) are rarely included in LGBTQIA+ provider training. Studies show this gap leads to negative healthcare experiences and worse healthcare outcomes for a-spec patients. It is important for Family Medicine Physicians (FMPs) to be aware of, validate, and provide care and resources for a-spec patients, in caring for patients of all ages, genders, and identity formations across the lifespan. We surveyed FMPs at UCLA Health to determine how various factors inform their comfort and knowledge relating to a-spec patients and to help inform future training.
Methods: In March 2025, we emailed an anonymous 34-question online survey to 252 FM attendings and residents at UCLA Health. 92 responses were collected and 5 excluded (2 repeats and 3 noncompleted). 5-point Likert scales assessed comfort, knowledge, clinical practice, normativity biases, and misconceptions relating to the a-spec community, both as specific a-spec identities (ace, aro, and agen) and as a group (a-spec). Results were quantified using descriptive frequencies and compared differences in comfort and knowledge relating to providing care for a-spec patients across comparison groups using chi-square and Kruskal-Wallis tests. Comparison groups were based on: Prior LGBTQIA+ training; Relationship to the LGBTQIA+ community; Exposure to a-spec patients; and Residency completion date.
Results: Most respondents were between 25-40 years old, White, female, attendings who finished residency within 5 years. 40.3% had a family member or friend in the LGBTQIA+ community and 19.5% identified as LGBTQIA+. Prior LGBTQIA+ training was associated with familiarity with ace and aro; Caring for > 1% a-spec patients was positively associated with comfort treating a-spec patients and addressing a-spec health concerns. LGBTQIA+ community ties were associated with preference to address a-spec concerns; and completing residency before 2020 with knowledge of breast cancer screening recommendations for agen patients. Respondents with LGBTQIA+ ties were more likely to be aware of ace microlabels and websites with a-spec information, while those recently finishing residency recognized aro microlabels.
Conclusion: Despite expressing overall comfort in caring for a-spec patients among attendings and residents, we found persistent deficits in a-spec training among UCLA Health FMPs. Knowledge gaps included confidence in defining a-spec terminology and familiarity with a-spec care guidelines. As comfort with and knowledge of a-spec patients were associated with exposure to the a-spec community, either through LGBTQIA+ community ties or prior care for a-spec patients, future training could incorporate patient voices to increase physician comfort and knowledge regarding a-spec identities and health concerns.
Pap Smears to Pulmonary Hypertension: A Mixed Methods Study Analyzing the Primary Care Experiences of People Who Use Stimulants in Los Angeles County
Authors: Aarushi Saharan BS (1), Jesse Clark MD (2) (3), Steven Shoptaw PhD (2)
Affiliations: (1) David Geffen School of Medicine at UCLA, (2) UCLA Department of Family Medicine, (3) UCLA Department of Medicine, Division of Infectious Diseases
Introduction: Methamphetamine related overdose deaths increased 333% in LA County from 2011 to 2021, and methamphetamine related ED visits increased 229% (SAPC 2024). Such a medically vulnerable population would benefit from increased utilization of patient centered primary care services (Dickson et al. 2021); however, few research studies have directly engaged with folx using stimulants around their access to, utilization of, and satisfaction in primary care services. This study hopes to bridge gaps in literature by conducting a mixed methods research study to understand the interactions of folks using stimulants with primary care services in LA County.
Methods: Participants were recruited from several syringe services programs in LA County. Inclusion criteria included: current stimulant use and residing within LA county. Exclusion criteria included: being under the age of 18 or being unable to speak English. Participants were first asked to complete a quantitative survey and were then asked to complete a semi-structured interview with the goal of 44 completed surveys and 20 completed interviews. Participants received a $50 visa gift card and a $100 Visa gift card at the end of survey and interview completion respectively. All quantitative survey data were analyzed descriptively using Microsoft Excel®. Qualitative interview data was analyzed inductively and deductively using thematic analysis (Braun & Clarke, 2006; Vaismoradi et al., 2013).
Results: Pending final data collection
Conclusion: Given the inductive nature of this study, it is hard to theorize the themes which may precipitate from this research; however, given previous qualitative studies conducted on similar subjects, we hypothesize that many participants will face burdens of navigation accessing care as well as previous stigmatizing experiences in primary care settings. Moreover, we anticipate that several participants will report positive experiences with primary care and we are particularly interested in evaluating participant engagement with mobile primary care modalities.
Impact of a Clinic-Based Medical-Financial Partnership (MFP) Program on Prenatal Health Utilization and Parental Quality of Life
Authors: Melanie Ramirez (1), Monique Holguin, LCSW, PhD (1, 2, 3), and Adam Schickedanz, MD, PhD (3)
Affiliations: (1) David Geffen School of Medicine at UCLA; (2) Harbor UCLA Department of Pediatrics; (3) Department of Pediatrics, David Geffen School of Medicine at UCLA
Introduction: Medical Financial Partnership (MFP) programs integrate financial support and services into clinic to promote health and well-being. The MFP at Harbor-UCLA (HUMC) evolved to provide a family-centered, whole-person health intervention by addressing financial and social drivers of health via 1-on-1 social work support for families in pediatric and prenatal care. Though the MFP has been shown to improve clinic visit show rates and vaccination rates in pediatric patients, its impact in prenatal patients is unknown. In this study, we assessed impacts of the MFP on prenatal care utilization and health-related quality of life for the first time.
Methods: The intervention was offered to expectant mothers in prenatal care (any trimester) planning to continue at the academic public medical center, HUMC, for their child’s pediatric care. We retrospectively compared 45 participants who opted into MFP to moms receiving usual care using 1-to-1 individual matching on mother/household demographics. Surveys were collected at baseline and every six months. Prenatal care utilization data were collected by chart review. Primary outcomes were prenatal care adequacy (Kotelchuck’s index of utilization) and Health Related Quality-of-Life (HRQoL, PROMIS-10) with mental and physical health sub-scales. We used descriptive statistics to assess participant characteristics and chi-square and adjusted linear and logistic regression to analyze outcome associations.
Results: Of 45 intervention participants enrolled in the MFP and 45 individually matched controls, 73.0% were Latino, 21.6% were non-Hispanic Black, and 5.4% were non-Hispanic White. English was the primary language for 73.6% and 72.1% had a high school education or less. Among intervention participants, HRQoL scores increased from baseline by 1.64 points at six months (p=0.13) and 2.19 at 12 months (p=0.11) of intervention. Similarly, mental health sub-scores increased by 2.38 points at month six (p=0.13) and 2.19 at month 12 (p=0.41), while physical health sub-scores increased by 1.63 points at month six (p=0.029) and by 4.72 at month 12 (p=0.023). Outcome measure analyses between the intervention and control groups are imminent and pending.
Conclusion: This is the first study to examine the impacts of the Medical-Financial Partnership model in a prenatal population. In the intervention group, HRQoL scores and physical and mental sub-scales all increased from baseline, with a dose-response relationship in HRQoL and physical health scores evidenced by a greater increase when comparing baseline to 6 and 12 month post-enrollment scores. We hypothesize that comparisons of MFP to control participants (forthcoming) will show that MFP enrollment is associated with a greater likelihood of having adequate prenatal care and increases in HRQoL scores.
Assessing Barriers to Medi-Cal Enrollment among Immigrant Communities in the Era of Medi-Cal Expansion in Los Angeles County
Authors: Jacqueline Cabral (1, 2), Alejandro Quiñones Baltazar (1, 2), Alejandra Rivas Deras (1, 2), Melissa Venegas (1, 2), Annie M. Hernandez, MD, MPH (1, 2), Ilan Shapiro, MD, MBA (3), Gerardo Moreno, MD, MSHS (1, 2)
Affiliations: (1) Department of Family Medicine at UCLA; (2) David Geffen School of Medicine at UCLA; (3) AltaMed Health Services
Introduction: Medi-Cal expansion efforts aim to improve access to healthcare for all adults, regardless of immigration status. The California Health Care Foundation reports 1.5 million undocumented people are currently enrolled in Medi-Cal. While the goal of Medi-Cal expansion is to increase enrollment among immigrant communities, research shows barriers still persist. Barriers may include language discordance, mistrust in healthcare, and policy misinformation. A review of the literature demonstrates limited research focused on understanding these barriers from the perspective of those on the frontlines: community stakeholders and healthcare providers.
Methods: We partnered with AltaMed, a federally qualified health center, to explore barriers to Medi-Cal enrollment. Together, we identified key stakeholders such as community health workers, enrollment specialists, clinicians, and legal experts. After iterative stakeholder meetings, insights from these discussions informed the development of an interview guide which will be used to conduct 20 semi-structured interviews, or until saturation is reached. Rapid community needs assessments will be conducted and interviews will be transcribed verbatim. A thematic analysis of data will be performed using a public health framework to explore barriers to enrollment (i.e., language, mistrust, administrative challenges), impact of policy on resource utilization, and effectiveness of community outreach.
Results: We anticipate themes around knowledge, trust, resource utilization, and efficacy of community outreach efforts will emerge. Limited awareness of Medi-Cal expansion and eligibility, misinformation on public charge, and budget cuts to local community organizations are expected to be identified as barriers to Medi-Cal enrollment among immigrant communities in Los Angeles county. We anticipate community stakeholders noting immigrant communities refraining from Medi-Cal enrollment due to fear of public charge and limited outreach efforts as a result of recent budget cuts at the state-level. We also expect a discussion of the need for increased training among community health workers on the policy implications of Medi-Cal enrollment among undocumented individuals to emerge.
Conclusion: Limited awareness of Medi-Cal expansion, language and technology barriers, and misinformation about public charge may impede Medi-Cal enrollment among eligible individuals. Mistrust in the healthcare system and government entities as well as administrative challenges likely further hinder enrollment. Budget cuts also affect community health programming and outreach to immigrant communities. We anticipate these findings will highlight the need for multilingual outreach, culturally tailored education, and stronger partnerships with trusted community organizations to improve enrollment efforts.
Steps Towards Healing: Assessing & Treating Wounds in the Skid Row Population
Authors: Kathleen M Kilroe, BS (1), Mary Marfisee MD, MPH (1, 2)
Affiliations: (1) David Geffen School of Medicine at UCLA; (2) Department of Family Medicine at UCLA
Introduction: Unhoused individuals are at an increased risk for acute and chronic wounds due to limited care access, poor hygiene, and environmental stressors. Consequently untreated wounds deteriorate and become infected, leading to chronic complications. Skid Row, a major homeless hub with ~4,000 individuals in Los Angeles, has a critical need for wound care that current safety-net systems struggle to meet. This study aims to investigate the nature of wounds commonly encountered on Skid Row, their etiologies, self-care practices, barriers to receiving care, and logistically, what resources are required to provide adequate street-medicine care.
Methods: Data was collected during weekly street medicine clinics held by the DGSOM Student Run Homeless Clinic ranging from 1-4 hours. Medical students directly walk through and provide care in Skid Row under the supervision of attending physicians. Clinics operate alongside leaders from Union Rescue Mission, an organization that offers patients low-barrier transitional housing. To identify best practices for launching a street-based wound care clinic, we administered mixed methods surveys to consenting patients (153). For each patient, we collected data on wound type, current care regimen, wound etiology, and barriers to care. Healthcare providers documented the supplies used to determine the minimum necessary resources for care. Descriptive statistics were used to evaluate the data.
Results: We found that 41% of triaged medical concerns were wound-related, with 66% of wound care patients being male (average age: 40.3) and 34% female (average age: 42.3). Chronic wounds (59%) were more prevalent than acute wounds (41%), with common chronic wound etiologies being traumatic (22%) and injection wounds (15%). Common acute wound causes include lacerations (27%), abrasions (22%). Barriers to care included self-management or delaying care (32%), lack of transportation/supplies (17%), fear of hospitals/law enforcement (15%), and responsibilities preventing care (15%). Most patients used tap water and cloth/plastic covers for wound care, and 76% felt they could self-care with supplies. The most used supplies were gloves, tape, gauze pads/rolls, soap, bacitracin, and adhesive bandages.
Conclusion: We have demonstrated a clear need for wound care in the Skid Row community given the significant number of patients with some variety of wound seeking care during outreach clinics. Our findings also highlight the importance of direct outreach with an established community partner given patient’s reported distrust of hospitals, various barriers to care, and an appreciable ‘wait and watch’ approach by patients. Finally, we found that street medicine wound care can be effectively provided with minimal supplies, however close follow up is needed.
Community Health Fair in San Diego
Authors: Samantha Williams, NP, Sophia Butler and Sophia Alvarez
Affiliations: University of California Los Angeles (UCLA)
Introduction: Community health fairs serve as a vital platform to promote public health awareness, provide preventive screenings, and connect individuals with local healthcare resources. This health fair, held in Southeast San Diego on April 19th, addresses public health needs, promotes health equity and positive health outcomes, strengthens community engagement, and connects community members to health resources and outcomes.
Methods: The event will feature multiple health-focused booths offering blood pressure screenings, glucose testing, BMI assessments, dental screenings, and nutritional counseling. We will offer Hands-only CPR and Narcan distribution. We will partner with local healthcare professionals, including physicians, physician assistants, and nurses, reach out to community partnerships, and engage directly with local organizations to ensure broad participation.
Results: Expected outcomes include increased awareness of chronic disease prevention, improved access to health resources, and greater community engagement in proactive healthcare. Data will be collected through participant surveys, tracking the number of attendees, screenings conducted, and referrals made for further medical care. Preliminary feedback will be analyzed to assess the impact and effectiveness of the fair.
Conclusion: The health fair is anticipated to enhance public health education, facilitate early detection of health risks, and strengthen community connections with healthcare providers. Insights gained from this event will help inform future initiatives aimed at improving community wellness and accessibility to preventive care.
“Movement Over Virtual Reality (MoVR)-Latinx:” Exploring the acceptability of a virtual reality (VR) dance-based exercise program among Latinos/a/x adults with prediabetes or at high risk of prediabetes
Authors: Desiree R. Acosta, MPH (1,2), Gael Perez, BS (2), Leslie Aguilar-Hernandez, BA (2), Iris Guzman-Ruiz, PhD (2), Michael Fine, BA (2), Josyel Castellon, MPH (2), Paulina Monteon-Garcia, MPH (2), Liana Gutierrez, BS (2), Jailene Cruz, BS (2), Gillian Gresham, PhD (2), Vanessa N. Torres, PhD, MPH (2), Yelba Castellon-Lopez, MD, MS (2)
Affiliations: (1) UCLA Underrepresented Minorities in Medicine Center of Excellence (UIM-COE), (2) Cedars-Sinai Cancer Research Center for Health Equity
Introduction: Physical inactivity is a significant public health concern contributing to various chronic diseases. Latina/o/x adults have higher rates of sedentary behavior compared to other racial and ethnic groups in the U.S. Despite evidence supporting the efficacy and growing adoption of VR exercise programs, little is known about the role they play in the Latina/o/x community. The purpose of this study is to assess the acceptability of a virtual reality (VR) dance program to promote physical activity among Latina/o/x adults with prediabetes or those at high risk of prediabetes in Los Angeles.
Methods: We conducted a qualitative study to explore the acceptability of a VR dance program. Participants (ages 18-70) who identified as Hispanic/Latino/a/x, spoke Spanish or English, and were diagnosed with prediabetes or identified as high-risk were recruited via snowball sampling and with the support of community health workers (CHWs). Participants were paired with culturally and linguistically congruent facilitators for a 10-minute VR Latin dance activity, followed by an in-person focus group (6-10 participants per group). The focus groups were organized based on language and on age range: 18-29, 30-49, and 50-70 years old.
Results: A total of 44 participants completed the focus groups (n=7), including 34 Spanish-speaking and 10 English-speaking Latino/a/x adults. Most participants were born outside of the U.S (82%), identified Spanish as the primarily language spoken at home (90%), and the average age was 45 (range = 18-72). Preliminary themes include: (1) positive reception of the VR experience, (2) learning new technology as a barrier to VR use, (3) assistance with technology use enhancing self-efficacy, (4) stress relief through VR, and (5) VR promoting physical activity by reducing the sense of judgment when exercising. This is preliminary data, with focus groups scheduled to continue until May 2025.
Conclusion: Results suggest that a VR Latin-based dance program may be acceptable for promoting physical activity and mental well-being among Latino/a/x adults with prediabetes or those at high risk. Based on our experience, providing guidance from bilingual/bicultural instructors will be essential for fostering engagement and encouraging uptake among Latino/a/x adults.
-
Transverse Myelitis with Negative MRI
Authors: Chandni Sakthi MS III (1), Andy Wu MS III (1), Zat Akbar Shaw MS III (2), Leopoldo Hartman MD, Basiru Omisore MD (3), Nariman Almnini MD (3), Harnek Singh MD (3)
Affiliations: (1) Kern Medical Center; (2) Rio Bravo Family Medicine in Bakersfield; (3) Clinica Sierra Vista at Bakersfield; (4) Department of Family Medicine at UCLA
Introduction: Transverse myelitis (TM) involves severe focal demyelination of the spinal cord. It is caused by autoantibodies that attack and damage sensory/motor neurons in the posterior/anterior horn of the spinal cord. Clinical manifestations include motor, autonomic, and sensory deficits. Many diagnostic tests such as CSF analysis and blood tests are effective in ruling in TM and expediting further management, but MRI is the main confirmatory diagnostic test. This report presents a case of TM where the patient experienced symptomatic relief, despite unremarkable thoracic and lumbar spine MRI findings.
Methods: A 41-year-old female with ovarian cancer and a partial gastrectomy was admitted for paraplegia and loss of sensation below the T2 dermatome. Two months earlier, she was hospitalized for bilateral lower extremity weakness, nausea, and vomiting, with normal cervical and lumbar spine MRIs. ANA and ANCA tests were negative. A month later, she was readmitted with paraplegia and sensory loss up to the xiphoid process, but MRIs(brain/thoracic/lumbar) remained negative. CSF showed elevated IgG (21) and proteins (58.1). She was diagnosed with Guillain-Barré Syndrome and received IVIG without improvement. During the current admission, she was bed-bound with incontinence and severe foot pain. Physical exam showed 5/5 strength in the upper extremities and 0/5 in the lower extremities, with decreased sensation below T2. Lumbar puncture showed elevated CSF IgG (9.9), while ANA, anti-aquaporin-4, and MOG antibodies were negative. Repeat MRIs were unremarkable. She received high-dose solumedrol, improving motor strength to 2/5, followed by plasmapheresis with mild recovery in strength and sensation.
Discussion: This case highlights a 41-year-old female with an extensive medical history, diagnosed with transverse myelitis (TM), despite atypical presentation and negative MRIs. While elevated CSF IgG and protein supported the diagnosis, multiple MRIs were inconclusive. The case highlights the difficulty of diagnosing TM when imaging is unclear, underscoring the need to integrate clinical symptoms, physical exam, and additional diagnostic markers. One key limitation was the lack of continuity in care, restricting long-term treatment assessment. Additionally, with initial evaluation, infectious or paraneoplastic etiologies like GBS or lung nodules which can mimic TM; weren't fully ruled out. Ultimately, a comprehensive, multimodal approach is essential for accurate TM diagnosis and timely intervention.
Suspected Penile Squamous Cell Carcinoma with Possible Metastasis: An Elderly Male Presenting with Persistent Penile Bleeding
Authors: Cameron Carlisle, MS IV (1, 2), Carol Avila Hernandez, MD (1), Nariman Almnini, MD (1), Ahamed El Azzih Mohamad, MD (1), Somotochukwu Nwebeh, MD (1), Hector Arreaza, MD (1)
Affiliations: (1) UCLA-Rio Bravo Family Medicine Residency Program; (2) Ross University School of Medicine
Introduction: In the US, primary malignant penile cancer accounts for 0.3% to 0.5% of male cancers. HPV is linked to 40% of cases, with squamous cell carcinoma making up over 90% of invasive types. Risk factors include smoking, lack of circumcision, phimosis, balanitis, lichen sclerosis, PUVA exposure, and low socioeconomic status. It mainly affects elderly men, peaking around 80 years. Metastasis to organs like the lungs, liver, or brain is rare but indicates advanced disease. We present an elderly male with suspected metastatic penile squamous cell carcinoma, a rare diagnosis challenging standard care.
Methods: An 82-year-old male with atrial fibrillation managed with Eliquis, diabetes, hypertension, and stage III chronic kidney disease presented with respiratory distress, weakness, and persistent bleeding from a penile lesion. Symptoms began five months earlier with a painless lump on the glans penis, later progressing to swelling and chronic bleeding. Initial foreskin biopsy was negative, and circumcision was performed, but bleeding persisted. CT imaging revealed multiple lung nodules, cavitary lesions, and a complex penile mass (13 x 4 cm). Pathology from the penile smear showed poorly differentiated malignancy, suspicious for squamous cell carcinoma. Given his declining health, surgical options were deemed unsuitable. Supportive care with IV antibiotics and oxygen was initiated, but his condition worsened, showing fluctuating confusion and respiratory distress. Due to advanced disease and poor prognosis, the patient was transitioned to comfort care and subsequently passed away. The diagnosis was based on pathology and imaging findings, suggesting metastatic penile cancer.
Discussion: Penile squamous cell carcinoma, though rare, often presents with bleeding and pain, with metastasis indicating advanced disease. In this case, delayed diagnosis and rapid progression led to suspected metastatic spread, indicated by lung nodules on imaging. Differential diagnoses included malignancy versus infection, but poor response to antibiotics supported malignancy. The rapid decline despite care was unexpected, highlighting challenges in managing advanced disease in elderly patients. Surgery was not pursued due to prognosis and comorbidities. This case underscores the need for early diagnosis. HPV vaccination, circumcision, and urologic evaluation are crucial to reduce cancer risk and improve outcomes. Early diagnosis and intervention are essential, especially in elderly patients.
Blast from the Past: A Forgotten Disease, Scurvy
Authors: Cameron Carlisle, MS IV (1,2), Zat Akbar Shaw, MS III (1,3), Yvette Singh, MD (1), Gagan Kooner, MD (1), Harnek Singh, MD (1)
Affiliations: (1) UCLA-Rio Bravo Family Medicine; (2) Ross University School of Medicine; (3) American University of the Caribbean School of Medicine
Introduction: Scurvy, caused by severe vitamin C deficiency, remains relevant in modern clinical practice, particularly among patients with malnutrition or altered gastrointestinal anatomy. Though rare, it persists in at-risk populations, including those with poor dietary intake, substance use, or bariatric surgery. U.S. data suggest a vitamin C deficiency prevalence of approximately 6–8% among adults. We present a case of a 52-year-old female with a history of gastric sleeve surgery, malnutrition, and non-healing skin ulcerations unresponsive to antibiotics, ultimately diagnosed with scurvy.
Methods: A 52-year-old female presented with painful, non-draining ulcers on her arms, legs, and buttocks for three months. Lesions began as vesicles that progressed into shallow ulcers. She had multiple scars from healed lesions and denied fever, chills, gingival bleeding, or joint pain. She received oral antibiotics during prior ER visits without improvement. History included gastric sleeve surgery, weight loss, poor oral intake, prior inhaled methamphetamine use, and smoking. She reported fatigue and difficulty maintaining nutrition due to early satiety and limited access to fresh food. On exam, she appeared cachectic with superficial ulcers and no signs of infection. Labs, including CBC, inflammatory markers, autoimmune panels, and infectious testing, were unremarkable. Due to chronic lesions and lack of response to antibiotics, other diagnoses, including pyoderma gangrenosum and cellulitis, were considered but ruled out. Given her risk factors, serum vitamin C was checked and found to be severely low. She was started on oral vitamin C 500 mg daily, with complete resolution within days.
Discussion: Scurvy remains underrecognized in modern practice, despite its potential to mimic conditions like pyoderma gangrenosum or cellulitis, leading to misdiagnosis and unnecessary treatments. In this case, the patient’s chronic, non-healing ulcers and lack of response to antibiotics raised suspicion for nutritional deficiency, especially given her history of gastric sleeve surgery, weight loss, poor intake, and substance use. The decision to check vitamin C was guided by these risk factors, ultimately confirming scurvy. This case highlights the importance of considering vitamin C deficiency in patients with unexplained ulcerations, especially when risk factors are present. Early recognition and supplementation can prevent morbidity and improve patient outcomes.
Towards Equitable and Long-Term Interdisciplinary Treatment of Patients With Illegal Silicone Injections and Chronic Foreign Body Soft Tissue Reaction
Authors: (1) Kushagra Tewari, (2) Levon Karamanoukian, (2) Lucas Karamanoukian, (3) Manuel Mendoza, MD
Affiliations: (1) David Geffen School of Medicine, UCLA, (2) Brentwood High School, (3) Department of Family Medicine, UCLA Health Toluca Lake
Introduction: Silicone biopolymers are non-FDA-Approved semi-solid to liquid fillers that are injected into soft tissue for cosmetic volumization of the face and body. Such illicit cosmetic fillers are often injected illegally into patients by non-medical practitioners who provide minimal informed consent regarding the short and long-term consequences of permanent fillers. Complications of treatment include foreign-body tissue reaction, chronic inflammation, filler migration, chronic edema, and granuloma formation, which are exacerbated by the marginalization of these patients in the clinical setting.
Methods: Patient 1: 38 year-old female with recurrent inflammation and pain in the legs. Several years prior, she received illegal cosmetic biopolymer injections into the buttocks and developed recurrent inflammation, skin color changes, infection, and soft tissue nodularity. Ultrasound imaging reveals diffuse infiltration of silicone biopolymer in the subcutaneous fat beyond the area of initial injection, despite attempts to surgically remove the material. Patient 2: 54 year old healthy female with complaints of chronic swelling, nodularity, and pain in the buttocks several years after receiving illicit injection of silicone biopolymers in Tijuana Mexico. Conservative management with corticosteroids and antibiotics failed to mitigate her symptoms. Ultrasound studies demonstrate diffuse infiltration of silicone biopolymer throughout the subcutaneous fat of the gluteal region with migration to adjacent anatomic regions including the sacrum and hips. The patient will require long-term medical management to mitigate long-term complications of chronic foreign body tissue reaction.
Discussion: Injectable silicone biopolymers of unknown provenance may induce chronic foreign body tissue reactions that have long-term health consequences. The United States Food & Drug Administration has issued multiple safety communiques regarding the potential short and long-term hazards associated with these illegal treatments used as dermal fillers. In addition to enduring the deleterious effects of chronic soft tissue reaction, patients who receive illegal silicone fillers often become marginalized by treating physicians because there are few mitigating solutions to reduce long-term health effects. Treatment of patients with liquid silicone complications should be equitable, non-marginalizing, and interdisciplinary with dialogue between surgical and non-surgical health care providers.
-
Self-Reported Cannabis Use among Patients Participating in Screening, Brief Intervention, and Referral to Treatment (SBIRT) for Risky Drug Use in FQHC Primary Care Clinics: The QUIT-Mobile Study
Authors: Alba Nunez, BS (1), Maria Vasquez, BS (1), Leticia Cazares, MPH (1), Lillian Gelberg, MD, MSPH (1), Dallas Swendeman, PhD, MPH (2)
Affiliations: (1) Department of Family Medicine, David Geffen School of Medicine, UCLA; (2) Department of Psychiatry and Biobehavioral Sciences, David Geffen School of Medicine, UCLA
Introduction: Self-reported substance use can be a practical measure in substance use (SU) assessments but may be limited by self-report biases such as recall errors and social desirability (underreporting). Biases may vary by context, retrospective recall periods, and over time. This analysis aims to compare multiple measures of self-reported cannabis use from adult FQHC primary care patients recruited for the QUIT-Mobile Study, an NIH/NIDA-funded screening and brief intervention trial aimed at reducing moderate risk drug use.
Methods: Participants (N=39) scored 4-26 on the WHO ASSIST, had cannabis as their Highest Scoring Drug (HSD), were randomly assigned to QUIT-Mobile intervention groups, were advised by a primary care provider (PCP) to reduce their HSD, completed two telephone health coaching (HC) sessions before the 6-month follow-up, and completed assessments at 3 and 6 months. PCPs reported motivation to reduce cannabis use. Self-reported cannabis use (CU) data for the past 3 months and 30 days were collected at enrollment, 3-month follow-up (3MFU), and 6-month follow-up (6MFU). CU in the past 14 days was assessed at HC Sessions. Consistency was checked by converting data to a 90-day timeframe and assessing differences within ±0.2 (18 days CU / 90 days).
Results: 78% of participants reported Past 3 Months (P3M) cannabis use (CU) consistent with Past 30 Days (P30D) CU at enrollment, 3MFU, and 6MFU. Over 6 months, P3M CU showed even distribution for low, intermediate, and high number of days CU, while P30D CU was more likely to be high or low. 24 participants were ready to reduce/quit CU, and 15 were not. P3M and P30D CU patterns were similar for people who were ready to reduce/quit and those who were not. Consistency between P3M and P30D CU increased by 6MFU. 38 participants completed HC Session 1 (S1) before 3 months, with 58% reporting P14D CU at S1 consistent with P30D CU at enrollment. 53% of participants not ready to reduce CU and 57% of those ready to reduce reported P14D CU at HC S1 consistent with P30D CU at enrollment.
Conclusion: Even with potential biases in self-reporting, the high rate of consistency between self-reported CU in the P3M and P30D suggests that participants provided reliable data on their CU across different time frames, potentially due to improved recall or better understanding of the reporting process. Self-reported SU across multiple time frames can be a useful tool in evaluating intervention effectiveness and tracking behavior change over time in clinical settings. Future studies might explore strategies to minimize biases or cross-validate self-reports with other measures to ensure accuracy.
Impact of Providing Medication Assisted Treatment and Psychiatric Pharmacology Lectures to Substance Use Disorder Counselors in Los Angeles Community-Based Clinics
Authors: Alexandra Hospodar, MD, Ololade Saliu, MD, Julio Meza, MD
Affiliations: Department of Addiction Medicine at UCLA
Introduction: In 2021, an estimated 2.5 million people aged 18 years or older in the U.S. had opioid use disorder in the past year, yet only 1 in 5 of them (22%) received medications to treat it (1). Research indicates that 43 percent of people in SUD treatment for non-medical use of prescription painkillers have a diagnosis or symptoms of mental health disorders (2). We sought to address potential barriers to medication-assisted treatment (MAT) for substance use disorders (SUD) and mental health treatment in hopes of increasing the number of patients who receive effective treatment for both SUD and mental illness.
Methods: We provided lectures focused on evidence-based medication treatment for both SUD and mental illness to a group of SUD counselors at Clinica Romero, a Los Angeles community-based clinic. We collected post-lecture surveys from SUD counselors to assess comfortability of explaining treatment options to patients and referring patients to services before and after the lectures were provided. We plan to examine number of referrals to MAT services and number of participants enrolled in MAT services pre and post lecture series at 2 different time periods- 1 month and 3 months post-lecture dates.
Results: We collected 21 post-MAT training surveys, and are in the process of collecting the post-psychiatric pharmacology lecture surveys. The MAT training survey results showed an overall increase in the comfortability of both explaining MAT to clients and referring clients to MAT services. We were also able to identify barriers that counselors continue to face when explaining MAT to their clients, with the number one barrier being clients not actually following up with the referral (48% of respondents). We also saw that 24% of respondents still have personal beliefs that MAT does not benefit their clients. We plan to start collecting number of MAT referrals and participants enrolled in MAT services within the next month.
Conclusion: This study highlights a need for more community education on MAT and psychiatric pharmacology. MAT lectures were seen to increase counselor comfortability with explaining and referring clients to MAT services, which may result in a higher number of individuals receiving life-saving treatment for SUD. We are interested to see if these findings are reflected on number of referrals/participants enrolled in MAT services, and if our post-psychiatric pharmacology surveys mirror similar results. Future research can be done to see if routine training or tailored workshops can provide further benefit.
Increasing Awareness of Palliative Medicine in the Hispanic Population in Pomona
Authors: A. Cortez, MD, S. Chung, MD,K. Tran, Do, C. Kwon, MD, J. Cheung, MD E. Roh, MD
Affiliations: Pomona Valley Hospital Medical center Family Medicine
Introduction: Palliative care is a specialty aimed at assisting people with serious illnesses by providing additional support to improve the quality of life for patients and family members. Unfortunately, many are not aware of the benefits of palliative medicine, often equating palliative medicine to hospice care. Even those who are aware of the specialty tend to have misconceptions about the services palliative care can provide. Our study is to educate Hispanic individuals in our local communities about palliative medicine to allow for appropriate access to this service in a timely manner.
Methods: We held educational sessions targeted towards a heavily Spanish-speaking Hispanic population in hopes to enhance their confidence in accessing services of palliative care. Knowledge and confidence regarding palliative medicine was assessed via the translated version of the Palliative Care Knowledge Scale (PaCKS) questionnaire before and after the session. PaCKS results before and after were primary endpoint and confidence level and free responses to barriers to palliative medicine were the secondary endpoint. Qualitative analysis was conducted on the PaCKS and confidence level data before and after sessions. A pattern thematic analysis was done for the free responses for barriers to palliative medicine.
Results: Our pilot study demonstrated a PaCKS pre-score average of 8.5 and a post-score average of 13. Maximum PaCKS score was 13. After t-test review, our p value was 0.4208.
After our educational session our participants provided feedback stating, "Why didn't I know about this when I had sick family members in the hospital", "If I would've known about it I would've used these resources"
Conclusion: We hope that by lowering the knowledge barriers and decreasing stigma regarding palliative medicine through our educational sessions, we will encourage participants and their friends and families to pursue more palliative care services in our local Hispanic population. We also expect that in future studies with a larger sample size we will be able to demonstrate greater significance in educational value.
Stitching Futures: Promoting Medical Careers Through Implementing Skill-Based High School Workshops
Authors: Amanda d’Almeida, MD, MPH, Paris Collier, MD, Spencer McCaffrey, MD, Ann M. Hernandez, MD, MS, MPH
Affiliations: UCLA Family Medicine Residency
Introduction: To describe the development, content, and implementation of a hands-on suturing workshop designed for high school students participating in a longitudinal pathway program.
Methods: Although the U.S. population is increasingly diverse, the physician workforce continues to lack proportional representation from underrepresented communities. Pipeline programs that offer early exposure to medical careers are critical for supporting youth from historically excluded backgrounds. The “Bridging the Gap” Pathway Program connects UCLA Family Medicine residents with high school students in the San Fernando Valley to provide mentorship and health education. To enhance student engagement and deepen understanding of medical practice, we introduced a hands-on suturing workshop, with future plans to integrate additional skill-based sessions featuring portable ultrasound and digital stethoscope technology.
Results: Family Medicine residents designed a 90-minute suturing workshop tailored to high school students with no prior clinical experience, using the Health Belief Model to promote self-efficacy, skill-building, and perceived relevance to future medical careers. The session included a brief didactic on wound care and suturing principles, followed by a resident-led demonstration and hands-on practice using synthetic skin pads and basic surgical tools. The curriculum emphasized technical skill development, clinical exposure, and confidence-building in a supportive and engaging environment. Informal feedback from students and resident facilitators indicated the workshop was a memorable and impactful component of the overall program.
Conclusion: Future Directions:
The workshop will be offered again during this academic year, with minor modifications based on facilitator observations and logistical considerations. Plans are underway to expand the hands-on curriculum to include portable ultrasound and digital stethoscope sessions, enabling students to explore diagnostic tools used in modern clinical practice.
Conclusion:
Hands-on clinical workshops represent a meaningful and scalable strategy for engaging high school students in medical education. As the program evolves, incorporating diagnostic
From Clinic to Code Blue: Tailoring POCUS Training for UCLA Family Medicine Residents
Authors: Harrison Lam MD, Amanda Tran MD, Monica Plesa MD, Anita Wong MD
Affiliations: UCLA Department of Family Medicine
Introduction: In 2023, the ACGME made point-of-care ultrasound (POCUS) training required for family medicine residents. UCLA Family Medicine Residency has since integrated POCUS workshops into core didactics. Beyond outpatient and inpatient care, UCLA family medicine residents uniquely serve as the rapid response and code blue team at their primary training hospital. This QI project focuses on the Fall 2024 workshop, which tailored content specific to each of these clinical settings. Pre- and post-surveys were administered to evaluate the effectiveness of the workshop and inform future curriculum development specific to residents within the program.
Methods: The POCUS workshop featured both didactic and hands-on teaching focused on volume status, pulmonary pathology, MSK landmarks (knee and shoulder), and first-trimester pregnancy. All participating UCLA family medicine residents completed a Google survey before and after the workshop. The survey included demographic questions on post-residency plans and utilized Likert scales to assess residents’ comfort with performing relevant POCUS scans across outpatient, inpatient, and rapid response settings. Pre- and post-workshop confidence at each station was also measured. Data was analyzed using frequency tables.
Results: A total of 14 family medicine residents (PGY1–PGY3) attended the POCUS workshop and completed both pre- and post-intervention surveys. All participants (100%) indicated their future career would include an outpatient setting, and 29% (4/14) also anticipated working in an inpatient setting. Prior to the workshop, only 50% (7/14) reported being able to perform at least one relevant ultrasound scan in the outpatient setting; this increased to 92% (13/14) following the workshop. The proportion of residents who felt capable of performing at least one ultrasound scan across all three clinical settings (outpatient, inpatient, and rapid response) increased from 29% (4/14) to 64% (9/14) following the workshop.
Conclusion: This workshop improved residents’ confidence in performing POCUS across clinical settings, with the greatest gains seen in outpatient care. Low baseline confidence in outpatient POCUS highlights a key gap in prior training yet also represents a high-yield area for curriculum development–particularly as all participants anticipate careers involving outpatient practice. Comparatively fewer residents both pre- and post-workshop felt confident applying POCUS in all three settings (outpatient, inpatient, and rapid response), suggesting the need for more comprehensive and longitudinal training.
Lessons from the Line: Student Research Coordinator Experiences when Recruiting Older Adults via Telephone for Clinical Research
Authors: Kaylee Hsieh, Stella Shebat, Felicity Nguyen, and Derjung Mimi Tarn, MD, PhD
Affiliations: Department of Family Medicine, David Geffen School of Medicine at UCLA, Los Angeles, CA
Introduction: Social isolation and loneliness are growing health concerns among older adults due to significant impacts on mental and physical health. While research often focuses on clinical outcomes, interactions between research coordinators and older patients offer valuable insight into patient lived experiences. The goal of this study is to describe student coordinator observations of telephone interactions with older adults when recruiting patients for a research study.
Methods: Student research coordinators made field notes of their experiences recruiting patients by telephone between March to April 2025 for a research study seeking to interview patients about a recent visit with their primary care provider. Telephoned patients belonged to community based physician offices around the country, and had to be 50 years of age or older, have Medicare insurance, and had an appointment with their primary care provider within the past 6-12 months. Field notes were analyzed using thematic analysis to identify major themes.
Results: This study is currently ongoing. To date, of 326 recruitment calls made, 7 of 134 (5.5%) patients who answered the phone engaged in more extensive conversation with a student research coordinator, ranging from 10 to 60 minutes. Six of these patients were female; 1 was male. Several expressed that they lacked social interaction at home and provided unprompted detailed information about their interactions with their healthcare provider. Several patients used the recruitment calls to express dissatisfaction with their medical care, though a few focused on their positive experiences. Personal life reflections were often shared. Coordinators noted that patients viewed these recruitment calls as an opportunity to engage in extended conversation rather than strictly discussing the study.
Conclusion: A subset of older patients contacted by student research coordinators attempting to recruit patients for a research study were eager to engage in prolonged interactions and revealed that they lack social interactions. These preliminary findings suggest a potential role for students to engage with older patients by phone to decrease social isolation and improve well-being.
Clinic Context Matters: Cultural and Operational Lessons from Implementing a Mobile SBI for Risky Drug Use
Authors: Luis Cortes, BA (1), Maria Vasquez, BS (1), Kelsey Ishimoto BS (1), Leticia Cazares, MPH (1), Lillian Gelberg, MD, MSPH (1), Dallas Swendeman, PhD, MPH (2)
Affiliations: (1) Department of Family Medicine, David Geffen School of Medicine, UCLA; (2) Department of Psychiatry and Biobehavioral Sciences, David Geffen School of Medicine, UCLA
Introduction: Digital Screening and Brief Intervention (SBI) programs offer scalable ways to address risky drug use, but success depends on more than technology. In safety-net settings, clinic workflows, patient trust, and cultural context shape engagement. The QUIT-Mobile Study tested a mobile SBI across FQHCs in Los Angeles using in-person and remote strategies. This analysis compares clinic models and explores how structural and cultural factors influence patient participation.
Methods: From April 2022 to March 2025, 19153 patients with upcoming primary care visits were invited to complete a mobile WHO ASSIST substance use screener. Clinics implemented either in-person workflows (with bilingual research assistants embedded in-clinic flow) or remote outreach via SMS to patients with scheduled primary care appointments. We analyzed screener initiation, completion, eligibility, and enrollment across clinic types. While outreach strategies differed, each clinic tracked engagement from the point of contact through enrollment. Participant-level data, including preferred language, were used to explore patterns of engagement and the role of cultural alignment in digital health delivery.
Results: In-person recruitment clinics showed higher variability in screener initiation (42.9% JWCH, 33.5% UMMA, 22.3% SCFHC) than remote recruitment clinics (39.6% Saban, 37.2% TCC). Completion also varied more at in-person clinics (74.4% JWCH, 55.7% UMMA, 36.6% SCFHC) than at remote recruitment clinics (51.9% Saban, 49.2% TCC). Clinic experiences suggest differences relate to waiting room time, completing screeners while roomed, and patient characteristics such as age and Spanish language preference. Bilingual study staff often support these patients to establish trust and improve comfort with self-administering screenings on tablets (iPads). Preliminary analyses explore associations between patient-level characteristics and screening initiation and completion.
Conclusion: While exploratory, preliminary findings and staff observations suggest lower engagement among Spanish-preferring patients. In-person recruitment settings enable bilingual, bicultural staff to build rapport and cultural connection, supporting stronger engagement than remote recruitment via text and phone. In communities where trust, language, and personal relationships guide care-seeking behavior, culturally responsive implementation is critical to scaling equitable digital health interventions.
Getting to The Clinic Door: Patient Perspectives of the 2024 Full Scope Medi-Cal Eligibility Expansion at a Safety Net Clinic in Los Angeles County
Authors: Miriam Ramos, MD MPH, Andree Franco-Safaie, MD MPH, Luisa Arevalo, MD, Martha Rodas-Maldonado MD, Maria Gonzalez MD, Fathima Sarah Nazarkhan MD
Affiliations: Harbor-UCLA Department of Family Medicine
Introduction: Federal changes to healthcare access in immigrant communities significantly affect L.A. County. In 2019, the “public charge” criteria were expanded to deny legal residency to immigrants based on healthcare utilization. Although the changes were rescinded in 2022, fear of “public charge” decreased enrollment in healthcare services. At the same time, in 2024, the eligibility criteria for Medi-Cal increased. In light of current policy, it is imperative to understand the perspectives of the 2024 Medi-Cal eligibility among patients served by the L.A. Safety Net to support enrollment in social benefits within a changing political climate.
Methods: This study aims to assess patient perspectives regarding the eligibility expansion of full scope of Medi-Cal so our clinic can improve patient services. Our study site is Lomita Family Health Center, part of the L.A. County Department of Health Services safety net that provides medical care to patients regardless of immigration or insurance status. We will use anonymous 10-question surveys to collect our data. Paper surveys will be administered in the clinic waiting room to patients 18 years old and older who speak Spanish or English over the course of 2-4 weeks until we reach our goal of 500 surveys. We will use qualitative analysis to generate descriptive measures.
Results: This project is in progress and does not yet have preliminary data. Since the patient population surveyed has already made it through the door of our safety net clinic, we expect to identify resiliency factors that permit patients to utilize healthcare resources despite the changing landscape of federal healthcare and immigration policy. Additionally, we anticipate that the survey results will provide an updated view of patient perspectives under the current federal administration.
Conclusion: This study will guide us on increasing awareness of the full scope of Medi-Cal eligibility expansion to our patients. This will help contribute to clinic-wide efforts to provide comprehensive primary care, including better support for our patients’ social needs.
-
Beyond Spinal Stenosis: Guillain-Barré Syndrome with Delayed-Onset Facial Nerve Palsy following Cellulitis in an Octogenerian
Authors: Belonwu Okafor, MD (1), Sylvester Okafor, MD (2), Arash Karimi Afshar, MD (1)
Affiliations: (1) Department of Family Medicine at Mission Community Hospital, California, USA; (2) Department of Family Medicine at Frontier Regional Hospital, Queenstown, South Africa
Introduction: Guillain-Barré Syndrome (GBS) is an acute autoimmune peripheral polyneuropathy often triggered by upper respiratory and gastrointestinal infections due to antigenic mimicry. Early bilateral facial nerve lesions are common, but delayed-onset unilateral facial nerve palsy is rare and occurs during the plateau or recovery phase. We present an 87-year-old male who developed GBS following right leg cellulitis, with a rare delayed-onset unilateral facial nerve palsy during the recovery phase. This is the first reported case of cellulitis as a possible trigger for GBS to the best of our knowledge.
Methods: 87-year-old male with chronic degenerative joint disease of the spine, who presented with a progressive neurological decline two weeks post-recovery from right leg cellulitis. Initial symptoms were sudden progressive ascending weakness and bulbar dysfunction. Patient was afebrile with a GCS score of 15, reduced power/muscle bulk/tone in both extremities, decreased tendon reflexes, and loss of proprioception. Laboratory results showed normal WBC, and non-reactive HIV, HBV, HCV and VDRL serologies. Chest X-ray showed homogenous opacities in the right lower lobe likely aspiration pneumonitis. MRI spine showed multilevel discopathies with mild cervical cord compression. CSF analysis was unremarkable. A diagnosis of acute inflammatory demyelinating polyneuropathy (AIDP), a common GBS variant, was made. Our patient met level 3 of Brighton diagnostic criteria. Treatment with IVIG and physical therapy were initiated. During the recovery phase, patient developed a right-sided facial nerve palsy with relapsed bulbar symptoms. Steroid therapy was initiated with a complete resolution of symptoms.
Discussion: The ascending sensorimotor deficits and bulbar dysfunction support AIDP, the most common GBS variant. MRI findings were incidental and did not explain the neurological symptoms. Protracted sepsis from cellulitis 2 weeks prior was the likely GBS trigger due to molecular mimicry and heightened inflammation, not aspiration pneumonitis following dysphagia from the GBS. Delayed-onset unilateral facial nerve palsy is rare and responds to steroids. This case underscores the importance of distinguishing GBS from structural spinal pathologies in the elderly, suggests cellulitis as a potential trigger, and emphasizes monitoring for delayed cranial nerve palsies. Further research should explore the role of soft tissue infections in GBS and steroid benefits on late-stage cranial nerve palsies.
A Curious Case of Chemical-Related Pneumonitis
Authors: Susan Li, DO, Ajinkya Mawley, DO, Shunling Tsang, MD, MPH
Affiliations: Riverside University Health System/ UC Riverside
Introduction: Vape-related chemical pneumonitis has emerged as a significant public health concern due to the increasing popularity of e-cigarettes and vaping devices, particularly among young adults. The inhalation of harmful chemicals, including flavoring agents, oils, and other toxic substances, can trigger severe lung inflammation, leading to respiratory distress and long-term pulmonary complications. As cases continue to rise, early recognition and management of this condition are crucial for preventing severe morbidity and improving patient outcomes.
Methods: A 32-year-old male with alcohol use disorder presented with 5 days of myalgia, fatigue, headache, congestion, and worsening dyspnea. He denied fever or rhinorrhea but admitted to vaping and marijuana use. He had received intramuscular Naltrexone 4-5 days prior. He works in the tattoo and piercing industry in California, with no recent travel, sick contacts, or environmental exposures. On exam, he was tachycardic, tachypneic, and hypoxic, requiring significant oxygen support. He had intercostal retractions and blunted breath sounds. Labs showed leukocytosis, eosinophilia, and lactic acidosis; HIV and respiratory panel were negative. Imaging revealed bibasilar/mid-zone opacities without pulmonary embolism. A mildly positive Fungitell raised concern for fungal infection, but bronchoscopy cultures were negative. Empiric antibiotics for pneumonia failed, so fluconazole was started for suspected coccidioidomycosis, with improvement within 2 days. On follow up 7 months later, repeat imaging showed near-complete resolution. He remains asymptomatic but continues vaping and marijuana use.
Discussion: Given acute respiratory symptoms, leukocytosis with uptrending serum eosinophilia, mildly positive Fungitell, and improvement with anti-fungal treatment rather than antibiotics, it is likely patient had some component of fungal infection, possibly from the vape product, inducing or exacerbating lung injury. However, the quick improvement is not as typical of a fungal infection. Another thought is, given naltrexone levels usually plateau in 2 weeks, which is when patient’s symptoms started improving, there could be an association with recent naltrexone injection as well. This case contributes to the current limited literature on chemical-related pneumonitis, specifically E-cigarette or Vaping use-Associated Lung Injury (EVALI) and naltrexone-related lung injury.
Beyond the Odds: A Case Study of Early Onset Pancreatic Cancer in a 32-Year-Old Male Without Risk Factors
Authors: Gerard de Guia, DO; Rahul Ahuja, DO
Affiliations: Department of Family Medicine at Dignity Health Northridge Hospital Medical Center
Introduction: Early-onset pancreatic cancer, defined as diagnosis before age 50, is rare but increasingly reported. Its high mortality underscores the critical need for early detection. This case describes a previously health 32-year-old male with no risk factors who presented with metastatic pancreatic cancer. The case highlights the importance of clinical vigilance, even in young, low-risk individuals.
Methods: A 32-year-old male initially presented to his primary care provider with back pain after lifting a heavy box at work. After a month, he developed classical symptoms of pancreatic cancer with unintentional weight loss, abdominal discomfort. vomiting, and diarrhea. Initial outpatient workup revealed mild anemia and elevated CEA. Imaging suggested a pancreatic mass, prompting referral to our center. CT Chest, Abdomen, and Pelvis demonstrated a 4.8 cm mass in the pancreatic body, innumerable pulmonary nodules, and lytic lesions of several vertebral bodies. Endoscopic ultrasound-guided needle biopsy (EUS-FNA) showed invasive adenocarcinoma. Despite expedited oncology referral and supportive care, the patient ultimately died from complications of pancreatic cancer.
Discussion: Early-onset pancreatic cancer is rare and often presents with nonspecific symptoms, leading to delayed diagnosis—especially in patients without identifiable risk factors. This case illustrates the need for clinicians to maintain a broad differential when young patients present with unexplained or progressive symptoms. Timely workup and specialist referral may improve early detection and potentially alter outcomes, even in seemingly low-risk individuals.
Daptomycin-induced Eosinophilic Pneumonia and Respiratory Failure in a Patient with Osteomyelitis
Authors: Lynn M. Utley, MD, Sara Larsen, MD, Tyler Goldberg, MD, Tina Barjasteh, MD, Monique George, MD
Affiliations: Kaiser Permanente Woodland Hills Family Medicine Residency Program
Introduction: Daptomycin-induced eosinophilic pneumonia (DIEP) is a rare medication adverse event that is characterized by eosinophilic infiltration of the pulmonary parenchyma. Presentations range from mild pulmonary infiltrates to severe respiratory complications. Herein, we present a male in his 70s receiving outpatient intravenous daptomycin for osteomyelitis who presented with fever and shortness of breath. The patient was ultimately diagnosed with DIEP, requiring cessation of daptomycin and initiation of systemic corticosteroid therapy.
Methods: A man in his 70s with a past medical history of diabetes mellitus type two and osteomyelitis of his left third toe, complicated by bacteremia, and on outpatient daptomycin therapy, presented for fevers and shortness of breath. Initial exam was notable for a temperature of 37.1 degree Celsius, oxygen saturation of 88% on room air, tachypnea, and crackles in the right lower lung. Laboratory evaluation revealed leukocytosis and an elevated peripheral eosinophil count. Imaging with chest x-ray showed new, scattered, patchy lung densities. The patient initially improved with standard treatment of community acquired pneumonia, however, he then began to clinically decline. C-reactive-protein at this time peaked at 269.3 mg/L. The remainder of the infectious workup was negative, despite prominent inflammatory markers. Bronchoalveolar lavage (BAL) was performed and revealed 76% eosinophils, which supported a diagnosis of DIEP. Daptomycin therapy was withdrawn and systemic corticosteroid treatment was started. The patient had significant improvement and was asymptomatic at follow-up.
Discussion: Daptomycin is an antibiotic that has an approved indication for the treatment of methicillin-resistant staphylococcus bacteremia. However, a potential adverse effect is DIEP. Often, the presentation of DIEP - fever, dyspnea, leukocytosis, and patchy opacities on chest imaging - suggests a leading differential diagnosis of multifocal pneumonia. However, elevated peripheral eosinophil count and failure to improve on empiric antibiotics should raise suspicion for DIEP. Diagnosis may be definitively supported with BAL. Prompt identification of DIEP is imperative, as failure to withdraw daptomycin, with or without corticosteroid therapy, may lead to serious negative outcomes, including death. This diagnosis must be considered in patients on daptomycin presenting with respiratory distress.
New Onset Lupus Myocarditis in a 27-year-old Female
Authors: Matthew Eli, DO; Amber Williams, DO
Affiliations: Department of Family Medicine at Dignity Health Northridge Hospital Medical Center
Introduction: A feared and potentially fatal manifestation of Systemic Lupus Erythematosus (SLE) is Myocarditis. Here, we present a case of a 27-year-old Female with an unremarkable past medical history who initially presented to the hospital with an incomplete Right Bundle Branch Block and elevated troponins. Her initial echocardiogram showed an Ejection Fraction of 30-35% along with a CT Angiography showing no signs of cardiac ischemia. Upon further lab work, she was ultimately diagnosed with Lupus Myocarditis.Her Myocarditis went into remission after the initiation of Mycophenolate Mofetil.
Methods: A 27-year-old Female with no past medical history was admitted for an incomplete RBBB and abnormal troponin elevation after presenting with new-onset fatigue and recovery from URI one week prior. During her hospital course, she had an echocardiogram that showed Heart Failure with Reduced Ejection Fraction of 30-35%. She subsequently had a CT Coronary Angiogram that showed patent coronary arteries. Autoimmune markers were positive for ANA speckled pattern with 1:640 ratio.
Outpatient, she performed a Cardiac MRI that was significant for abnormal biventricular subendocardial late gadolinium enhancement (LGE) and patchy LGE of papillary muscles. This was consistent with myocarditis related to subendocardial fibrosis as well as clinical suspicion for Giant Cell Myocarditis. She underwent endomyocardial biopsy, which resulted in diffuse nonspecific inflammation and ruled out Giant Cell Myocarditis. Her Myocarditis went into remission with the initiation of Mycophenolate Mofetil, with subsequent Echocardiogram showing Ejection Fraction of 45-50%.
Discussion: SLE is a complex connective tissue disease that can potentially affect every organ of the human body. It can have cardiac manifestations and, if present, is associated with increased morbidity and mortality. The purpose of reporting this case is to highlight that Lupus Myocarditis should remain on the differential for a patient of younger age with no prior cardiac risk factors, particularly if the patient is a female of childbearing age. If an EKG is abnormal, it is reasonable to order a troponin-I level to determine if myocardial injury is present. If an autoimmune etiology is on the differential, it is imperative to start immunosuppressants as soon as possible to prevent morbidity and mortality from damage to the various structures and functions of the heart.
Refractory Delirium Tremens: Beyond Benzodiazepines
Authors: Sabrina Wedee, DO, and Sabrina Afroz, MD
Affiliations: Department of Family Medicine at Mission Community Hospital
Introduction: Delirium tremens (DT) is a life-threatening complication of alcohol withdrawal, affecting 3-5% of chronic alcohol users. This case highlights a 41-year-old male with alcohol use disorder who developed refractory DT unresponsive to high-dose benzodiazepines, requiring escalation to multimodal sedation with phenobarbital, propofol, and midazolam. Though rare, refractory DT poses significant management challenges and increases mortality risks if not promptly recognized and treated. Early identification and aggressive treatment are crucial in severe alcohol withdrawal.
Methods: A 41-year-old male with a history of diabetes, hypertension, and chronic alcohol use (5–6 drinks daily for 8 years) presented to the ED with chest pain, diaphoresis, tremors, and agitation. He reported auditory hallucinations, paranoia, and believed people were planning to harm him outside of his work. On arrival, he was hypertensive (BP 179/117), tachycardic (HR 130), afebrile (T 97°F), and saturating 96% on room air. Labs showed ethanol 21 mg/dL, and his electrolytes were within normal limits. The CIWA score on arrival was 25. Despite escalating benzodiazepine doses (lorazepam and diazepam), his agitation worsened, leading to intubation and sedation with a propofol drip. A phenobarbital loading dose and midazolam drip were also added. Imaging and labs ruled out other causes. The patient was stabilized with multimodal sedation and transferred to the ICU. He required multiple days of ICU-level care before gradual weaning of sedation was possible.
Discussion: Refractory DT, or severe alcohol withdrawal unresponsive to high-dose benzodiazepines, presents major challenges due to altered GABA receptor sensitivity. In this case, despite substantial benzodiazepine use, the patient’s symptoms escalated, requiring multimodal management. Phenobarbital can be beneficial when combined with benzodiazepines due to synergistic effects: benzodiazepines increase the frequency of GABA channel opening, while barbiturates increase duration. Propofol is also effective, as it can open chloride channels independently of GABA and inhibit excitatory neurotransmission. Early recognition of refractory DT is crucial to prevent morbidity and mortality, which can reach 37% without treatment.This case highlights the need for prompt escalation and individualized treatment.
An Uncommon Cause of Hemolytic Anemia: Vitamin B12 Deficiency in a Young Adult Female
Authors: Nick Hu, MD, Lara N. Garcia, MD
Affiliations: Kaiser Permanente Los Angeles Medical Center Department of Family Medicine
Introduction: We present the case of a 29-year-old female with no significant past medical history who reported a one-month history of upper respiratory symptoms and progressive yellowing of the skin. Laboratory evaluation revealed findings consistent with hemolytic anemia. Further workup identified a severe vitamin B12 deficiency as the underlying etiology. The patient's condition improved rapidly with vitamin B12 replacement therapy, avoiding intensive interventions typically associated with hemolytic disease. This case highlights an uncommon but important cause of hemolysis and underscores the need to consider vitamin B12 deficiency in the differential diagnosis of hemolytic anemia. This case highlights the role of early screening for B12 deficiency in patients presenting with signs of hemolysis.
Methods: A 29-year-old female with no past medical history presented to urgent care with a one-month history of fatigue, upper respiratory symptoms, and progressive yellowing of the skin. She denied fever, weight loss, bleeding, or abdominal pain. On physical examination, the patient was hemodynamically stable. She was alert, pale, and had scleral icterus and jaundice. No hepatosplenomegaly or lymphadenopathy was appreciated, and there were no signs of active bleeding. Upon admission to the inpatient hospital patient with laboratory results revealing pancytopenia with, wbc 3.3, macrocytic anemia with hgb 7.2 and MCV 118, and platelet of 46. Additionally, haptoglobin < 4 mg/dl, LDH of 1030, Total Bilirubin 3.7 mg/dl, Direct bilirubin 0.5 mg/dl, reticulocytes of 2.5%, negative direct combs, Vitamin B12 <146, with positive intrinsic factor. No schistocytes on peripheral smear. Patient was started on three times a week vitamin B12 intramuscular injections with subsequent improvement in pancytopenia with Hgb 11.2, WBC 7.5 and Platelets 478 and resolution of symptoms.
Discussion: This case illustrates a rare and underrecognized presentation of vitamin B12 deficiency, manifesting as hemolytic anemia with pancytopenia. While megaloblastic anemia is the classic presentation, intramedullary destruction of red blood cells due to ineffective erythropoiesis can lead to a pseudo-hemolytic picture, including elevated LDH, indirect hyperbilirubinemia, and low haptoglobin. Unlike peripheral hemolysis, no schistocytes or positive Coombs test are found.
Early identification is critical, as delay in treatment may result in irreversible neurologic damage or require interventions such as corticosteroids, transfusions, or extensive diagnostic procedures. This case advocates for routine evaluation of B12 levels in patients presenting with unexplained cytopenias and hemolysis.
-
Evaluating the Impact of Routine Follow-up Phone Calls on CPAP Adherence Rates in Patients with Sleep Apnea
Authors: Mercy Azubuko-Udah, M.B.B.S., Zaki Elmaghraby, MD, Sayaka Tokumitsu, MD, Kevin Kemp, MD, Heather Wynne, MD, Melissa Tejada MD, Mischelle Nelson, MD, Oliver Ting, MD
Affiliations: Department of Family Medicine Charles R Drew University; Martin Luther king Outpatient Center
Introduction: There is a more than 3 fold increase in all-cause-sudden death and Cardiovascular mortality in individuals with untreated Severe Obstructive Sleep Apnea (OSA) . First line management for OSA is with Continuous Positive Airway Pressure Machine(CPAP).
A JAMA Meta-analysis from October 2023, “ Adherence to CPAP treatment and Risk of recurrent Cardiovascular Events” concludes that efficient CPAP use is clearly important for risk reduction of Cardiovascular and all cause morbidity and mortality .
The aim of this QI Project was to find out if the discouraging nature of CPAP adherence can be improved with regular follow up phone calls.
Methods: A multidisciplinary team consisting of Residents, Respiratory Therapists and Sleep Medicine Physician was assembled for this project in Martin Luther King Outpatient Center.
40 patients were randomly selected, ages 32-67 years old with a mean age of 50. Baseline compliance reports data was collected. A team of Residents made phone calls on month 0, 3 and 6 in order to identify factors associated with low adherence or compliance rates and areas of improvement of the current management process. During the focused phone appointments, patients were educated on pathophysiology of OSA, counselled on benefits of CPAP use and possible consequences of non-adherence.
Follow up compliance rates were collected to assess the impact of the implemented intervention at subsequent months .
Results: A total of 40 participants were evaluated(22 men, 18 women).Factors associated with low CPAP adherence were the common ones such as Poor mask fit, air leaks, nasal congestion, dryness or discomfort and claustrophobia. The participants who needed CPAP machine parts changed or fixed were connected with Respiratory therapists who followed up with them and made the necessary changes.
At the end of the 6 month period, there were only 24 active patients out of 40. 16 patients discontinued use of CPAP or were unreachable for 4 consecutive months. Mean compliance rate was 52.2% in these 24 patients. 14 patients out of 24 active patients had at least a 50% or more decline in adherence rate. 8 patients maintained similar adherence and only 2 patients had significant improvement in CPAP compliance.
Conclusion: CPAP remains the most effective management for OSA, even with several newer therapies, devices and surgical options available now. Our project suggests that despite several phone calls, changes to machine parts like masks, tubing and better access to the Sleep Medicine Clinic and Respiratory therapists; CPAP adherence continues to be a problem for many patients with OSA.
The Effects of Prescribing Exercise on Patient Health: The Park Rx LAC Project
Authors: Mevan Happawana, MD (1), Eloisa Gonzalez, MD (2); Aleesha Shaik, MD (2); Tony Kuo, MD (2); Kyla Sherwood, MD (2); Rebecca Reeves PT, MPT (2), Samantha Bonilla MPH (2)
Affiliations: (1) Department of Family Medicine UCLA; (2) LA General Medical Center & Olive View-UCLA Medical Center in relation with Los Angeles County Department of Public Health
Introduction: How many times have you advised a patient to exercise and then left it to them to do the leg work with poor to no results. Given that exercise is one of the most important aspects of everyone's health, what if we could just prescribe it? The journal SJM&SS provides evidence for prescribing exercise as therapy in 26 different chronic diseases, including psychiatric, neurological, metabolic, cardiovascular, pulmonary, musculoskeletal, and cancer. Further expansion of this type of data and a more direct and controlled method of implementation (LA based) is a novel idea and what we are looking to pilot with the Park Rx LA County Project.
Methods: The Park Rx LAC is a 2 year initiative aimed at patient overall health involving physicians at LA General Medical Center, Olive View-UCLA Medical Center, local universities, and community parks. DHS clinicians will refer patients to kinesiology student led physical activity programs offered at two local parks. The One Degree app will be used for physicians to monitor patient attendance. Survey responses will be collected via Microsoft Forms. Patients provide a HIPPA consent form for access to progress notes, labs, discharge summaries. Parameters being evaluated are to be determined but will likely include things such as mood, blood pressure, weight, etc. Current data is pending as the project is in it’s early phases. Statistical analysis is to be determined based on upcoming collected data.
Results: Pending
Conclusion: Park Rx LAC is an innovative initiative starting to collect data on the effects of prescribed exercise on patient populations. In the upcoming months, continued efforts will focus on patient and physician recruitment, continuing data collection, and finalizing written partner agreements. Although in the early stages, further expansion of such projects could have significant lasting impacts in how we practice healthcare.
Student Run Los Angeles
Authors: Joseph Coppiano, MD (1), Emily M. Miller, MD (2, 3, 4), Sydnie Vo, MD (5), Frances Tao, MD, MPH (5), Kuan-Ting Chen, MS (6), Nicholas J. Jackson, PhD, MPH (6), Alan Grusky MD (7), Christal Clemens MD (7), Phallaraingsey Chhay MD (7), Leah Wildmann8, Summer Bloom, ATC (2), Joshua Goldman, MD, MBA (2, 3, 4)
Affiliations: (1) University of Alabama, Birmingham, Division of Sports and Exercise Medicine, Department of Family & Community Medicine, (2) University of California, Los Angeles, Division of Sports Medicine, Departments of Family Medicine and Orthopaedic Surgery, (3) The Luskin Orthopaedic Institute for Children, Center for Sports Medicine, (4) University of California, Los Angeles, Department of Intercollegiate Athletics, (5) University of California, Los Angeles, Department of Medicine, (6) University of California, Los Angeles, Department of Medicine Statistics Core, David Geffen School of Medicine, (7) University of California, Los Angeles, Department of Family Medicine, (8) University of California, Los Angeles
Introduction: Objective: Little data exist on the impact of strength training on injuries in adolescent marathon runners. The purpose of this study was to determine if a standardized strength training program led to a decrease in injuries in adolescents training for a marathon.
Design: Prospective cohort study
Setting: 194 high schools participating in Students Run Los Angeles
Participants: 608 adolescents ages 12 to 19
Interventions: Schools in the strength training group (STG) completed a standardized strength training program twice a week over the 26 week course of marathon training while the control group (CG) followed traditional training protocol.
Methods: SRLA coaches from 194 schools voluntarily signed up to have their teams participate in this research study before the start of the 2022-2023 training season (Figure 1). Once a coach agreed to participate, parental consent and adolescent assent were collected from each participant. Coaches from each school were given the option to join either the strength training group (STG) or the control group (CG) before the season commenced. The STG was provided with a structured strength training program to be completed twice a week, and instructional videos detailing the exercises were made available to coaches. Coaches were instructed to perform the strength training program twice a week for the duration of the training season. Coaches in the CG were not provided the structured exercises.
Results: There was not a statistically significant difference in a specific location of injury. We hypothesize that the current data supports that strength training in adolescent runners may not specifically prevent one type of injury but rather better prepare the runner for the long training season.
Conclusion: Altogether, our results support that our standardized strength training program could help reduce injuries during the training season and increase the likelihood of completing the marathon. This protective effect was seen strongest in female runners who had lower injuries reported with increased weekly mileage. Despite having similar overall injuries reported, males who completed our program were able to have a higher overall weekly mileage.
Novel Palliative Care Curriculum and Clinical Experience Pilot within a Family Medicine Residency
Authors: Savreen Saran, MD (1), Annie Phung, DO (2), Olivia Wu, MD (1), Patrick Samones, MD (1), Timothy Weiss, MD (1), Shannon Bell (2), Teresa Khoo (2).
Affiliations: (1) Department of Family Medicine at UCLA; (2) Department of Palliative Medicine at UCLA
Introduction: Effective July 1 2023, new family medicine residency requirements per ACGME included understanding how to communicate goals of care, including end-of-life goals and pain management, and exposure to pain management as core competencies for graduation. These new requirements do not specify explicit experience within the field of palliative medicine to address end-of-life conversations and pain management. At a large academic tertiary medical center, our family medicine residency program piloted a novel curriculum to approach the new requirement, including specialized lectures, outpatient rotation exposure, and a communications workshop.
Methods: Novel curriculum development at a single large academic center was designed to fulfill the new ACGME requirements through an integrated approach within the field of palliative medicine. Anonymous surveys using Qualtrics were sent to all UCLA family medicine interns from August 2024 - June 2025 to assess perceived comfort in palliative care topics before and after exposure to a one-year primary palliative care curriculum including: 1-week outpatient clinical experience, yearlong series of educational lectures, and a formalized communications workshop. This study specifically focused on the evaluation of palliative topics before exposure to the curriculum through the aforementioned Qualtrics survey.
Results: Our presurvey results demonstrate that the majority of the residents were familiar with the scope of palliative medicine, they did not feel prepared to discuss and apply topics related to the field. No resident agreed with feeling comfortable identifying and managing common signs and symptoms of patients nearing death. The large majority did not feel comfortable with pharmacologic pain management with opioid prescription, dosing, or side effect management. A majority of residents also did not feel comfortable with delivering difficult news, discussing goals of care, managing psychosocial distress, end-of-life protocols. However, a majority of residents felt comfortable identifying when to refer a patient to palliative medicine.
Conclusion: Our preliminary results suggest that PGY1 family medicine residents lack experience and comfort in end-of-life goals, conversations, and symptom management that would benefit from intervention. Our piloted curriculum design could increase resident confidence in symptom management and communication within the field of palliative medicine. This novel curriculum will continue to integrate results and feedback into the curriculum and follow the PGY1 residents longitudinally to assess adequate training in addressing end-of-life care.
Perspectives on Burnout in Early Career Primary Care Physicians Caring for Under-Resourced Populations
Authors: Saya Yusa, MD (1); Yalda Jabbarpour, MD (2); and Derjung Mimi Tarn, MD, PhD (1)
Affiliations: (1) University of California Los Angeles, Los Angeles, CA, (2) Robert Graham Center for Policy Studies in Family Medicine and Primary Care, Washington, DC
Introduction: Existing literature on physician burnout focuses primarily on resident physicians or does not distinguish how long physicians have been in the workforce. There is limited research on burnout in recent residency graduates and in those who provide primary care in under-resourced settings. This study aims to explore the prevalence of burnout in recent residency graduates who practice primary care in under-resourced settings, to understand the factors that contribute to and mitigate burnout from the perspective of these physicians, as well as to assess their likelihood of long-term retention in providing primary care in under-resourced settings.
Methods: One-time semi-structured interviews were conducted with primary care physicians who recently graduated from residency and work in under-resourced communities in California to assess motivations for pursuing a career in primary care and working with under-resourced communities, burnout factors, burnout mitigators, and retention. Participants provided information on their demographics, workplace characteristics, and level of burnout (measured by the Mini Z Burnout Survey). Interviews will be analyzed using thematic analysis.
Results: We have 27 participants and will describe their demographics, workplace characteristics, and level of burnout. Analyses are in progress, and preliminary analysis suggests that half of the participants were of a racial or ethnic group that is underrepresented in medicine. Another theme is that most participants addressed their burnout by decreasing their hours doing direct primary care. Analyses will describe physicians’ perspectives about staying in their current position or role and continuing to care for under-resourced patients. We expect additional analyses to reveal physician motivations for working with under-resourced patient populations, their experience and satisfaction working with these populations, and thoughts they have on how to address physician burnout.
Conclusion: This study will generate insights on the unique factors influencing burnout, its mitigators, and the motivations behind why these recent physician graduates are working with under-resourced populations. It also examines the factors that impact retention and the likelihood of these doctors continuing to do primary care in these settings. The results are expected to inform actionable strategies for reducing burnout and enhancing workforce sustainability in these settings, as well as the development of targeted interventions to address the primary care workforce crisis in vulnerable populations.
Enhancing MSK Education: A Quality Improvement Initiative Using the MSK Guide for Medical Students
Authors: Connie Oh, MD; Shane Hervey, MD; Marissa Vasquez, MD, MBA
Affiliations: UCLA Department of Family Medicine, Division of Sports Medicine
Introduction: Musculoskeletal (MSK) complaints are a leading reason for medical attention in the U.S.1 However, medical students often lack the knowledge and confidence to perform MSK exams. 2 In addition to hands-on instruction, structured reference materials such as handouts may improve student learning and retention. This quality improvement project aims to enhance medical students’ MSK exam skills by providing concise, curated handouts following MSK teaching sessions for referencing throughout their Family Medicine clerkship.
Methods: Second- and third-year UCLA medical students were recruited during the MSK teaching session at the start of their Family Medicine clerkship. Using a 5-point Likert scale, participants completed a pre-intervention survey assessing their confidence and knowledge in performing MSK examinations. Following a didactic session, students received electronic copies of the MSK exam to reinforce key concepts and promote continued reference throughout the rotation. At the conclusion of the clerkship, a post-survey was administered to reassess their knowledge and confidence in performing MSK examinations. Mean confidence scores pre- and post-intervention were recorded. The paired Student’s t-test will be used to assess the significance of changes in confidence and accuracy.
Results: Eighteen pre-intervention survey responses were collected. Using a 5-point Likert scale, students self-reported comfort with the overall MSK exam (mean 2.38), the shoulder (2.27), knee exam (2.55) and ankle exam (2.11). Students answered a short clinical question with correct responses rates of 44.4% for shoulder, 38.8% for knee and 33.3% for the ankle. The most frequently reported online resource used for MSK exam knowledge was YouTube (55.5%). Post-intervention data, including comparative analysis with pre-intervention results is currently pending and expected to be available for presentation.
Conclusion: There is an observed gap between self-perceived confidence level and performance on the knowledge questions. This suggests a disconnect between confidence and actual MSK understanding. While there is a plethora of online resources available, their reliability may be unclear to novice learners. To address this, our project aims to provide a vetted MSK learning guide to support and enhance student’s learning during their Family Medicine clerkship. The guide also promotes students to engage in self-learning by utilizing curated resources.
Under Pressure: The Relationship Between White Coat Hypertension and GAD-7 Scores
Authors: Genevieve Tusa, D.O., MPH; Cindy Yang, M.D.; Lucy W. Lee, M.D.
Affiliations: Dignity Health Family Medicine Residency Program at Northridge
Introduction: Hypertension is a widespread health concern, influencing the lives of millions globally. Of these individuals, a notable subset report normal blood pressure when measured at home; a phenomenon known as white coat hypertension (WCH). This condition is thought to be influenced by psychological factors, with studies suggesting that 30-50% of patients with WCH report symptoms of anxiety. This study aims to investigate the correlation between anxiety and elevated blood pressure readings in the office setting. By better understanding this relationship, this research seeks to improve hypertension management and patient outcomes.
Methods: This is a prospective observational study conducted in an outpatient Family Medicine office. Inclusion criteria includes patients aged 18 or older with elevated blood pressure readings and who report their blood pressure is typically higher at the doctor’s office. Those who qualify complete a GAD-7 questionnaire and a brief demographic survey.
Results: Data collection is currently in progress. The primary analysis will explore correlations between elevated blood pressure in the office and GAD-7 scores. Statistical methods will include comparisons of mean blood pressure and anxiety scores, with P-values used to assess significance. Additional analyses will examine demographic and lifestyle factors that may influence the relationship between anxiety and blood pressure readings.
Conclusion: In this study, we hypothesize that screening positive for white coat hypertension (WCH) will positively correlate with higher anxiety scores. Preliminary findings will help determine whether anxiety, as measured by the GAD-7, contributes to elevated blood pressure readings in the office setting. Limitations of the study include its observational design, potential self-report bias, and the projected small sample size. Results are pending and will be further analyzed once data collection is complete.
4-Week Shoulder Ultrasound Curriculum: A Quality Improvement Project
Authors: Jeremy Swisher, MD, Marissa Vasquez, MD, MBA
Affiliations: UCLA Division of Sports Medicine
Introduction: Primary care physicians frequently manage musculoskeletal (MSK) conditions, yet many lack formal MSK ultrasound training, leading to low confidence. While ultrasound is a valuable tool for diagnosis and procedures, barriers such as limited time, equipment, and trained faculty hinder education. Structured learning can help bridge this gap. This quality improvement project implemented a 4-week diagnostic MSK ultrasound curriculum focused on the shoulder for family medicine residents, using a flipped-classroom model with pre-session materials and weekly hands-on workshops.
Methods: This 4-week shoulder MSK ultrasound curriculum combined self-directed learning with hands-on workshops. Through a flipped-classroom model, learners reviewed curated materials, including custom slide decks on shoulder anatomy with a voiceover, scanning protocols, normal ultrasound images, and selected high-yield AMSSM videos. Weekly 1.5-hour in-person sessions allowed participants to practice on live models with real-time guidance from a sports medicine physician. Each session focused on specific components of the shoulder exam. Two portable machines and existing clinic tools were used. Learners completed pre/post quizzes, confidence ratings, and provided feedback via surveys and discussion.
Results: Learners demonstrated a significant increase in shoulder ultrasound knowledge following the intervention. The mean score on a 10-item quiz rose from 5.67 to 9.00. Notable improvements included accurately identifying rotator cuff tendon insertions and recognizing optimal probe positioning. Confidence ratings (Likert 1–10) increased from 4.14 to 7.75, an 87% improvement. Participants reported greater ease with transducer handling, image optimization, and systematic scanning. Hands-on practice was unanimously described as the most valuable component, while many noted the flipped-classroom format enhanced engagement. No adverse events occurred, and only minor scheduling adjustments were needed.
Conclusion: This project demonstrates that a focused, structured curriculum can address MSK ultrasound training gaps. The flipped-classroom model proved efficient, maximizing hands-on practice and likely accelerating learning. Alignment with the AMSSM checklist ensured that participants learned a standardized approach to the shoulder exam. Notably, confidence rose by 87%, which is crucial for clinical use. Supervised repetition helped demystify the ultrasound machine and imaging process for the learners. Future studies could assess if confidence leads to continued independent use and skill retention.
-
Fatigue, Irritable Mood, and Decreased Libido as Presenting Symptoms of a Sellar Brain Mass in a 22-Year-Old Male
Authors: Connor Gehris, MD, Olajumoke Idris, MD, Kapua Meyer, MD, Daniel Lee, MD
Affiliations: UCLA Department of Family Medicine, Family Medicine Residency Program
Introduction: Many men are presenting to their primary care physicians with symptoms of fatigue, irritable mood, and decreased libido – and requesting their testosterone level checked. It can be difficult to determine when hormonal workup is indicated. While the Endocrine Society does not recommend screening asymptomatic males, it is recommended to check males with symptoms that may be consistent with decreased testosterone levels. In this case, we describe a patient with symptoms of fatigue, irritable mood, and decreased libido and the importance of working up androgen deficiency in a timely manner.
Methods: A 22-year-old male presented in 11/24 for evaluation of low energy, irritable mood, and decreased libido of six-month duration. Work-up on initial presentation was significant for normocytic anemia (hemoglobin 11.4), neutropenia (988 cells/uL) and low total testosterone (73 ng/dL). Both an endocrinology referral and further anemia workup were ordered. While on vacation in 12/24 in Brazil, the patient had a CT Brain done for new onset headaches. This showed a pituitary mass. At this time, he also had low thyroid hormone, cortisol and again low testosterone levels on serum workup. These symptoms persisted upon return to the USA where he began to experience left temporal visual field loss. MRI of the pituitary revealed a giant multilobulated cystic lesion of the sella and the left cavernous sinus/SOF most suggestive of Rathke’s cleft cyst. Patient saw endocrinology and neurosurgery and is now status post transsphenoidal resection of a cystic pituitary lesion that appears to be a mixed Rathke’s cleft cyst/craniopharyngioma.
Discussion: Fatigue, irritable mood, and low libido can be common presenting symptoms in the primary care setting. While there are many causes of this constellation of symptoms, it is important to consider secondary hypogonadism as a contributing factor among post-pubertal aged males. Including serum testosterone levels in an initial diagnostic workup may lead to this diagnosis of secondary hypogonadism. In this case, the cause of the patient’s androgen deficiency was a mixed Rathke’s cleft cyst/craniopharyngioma. Both are benign lesions that are typically located in the sellar and suprasellar or parasellar regions and can cause endocrine deficiencies, visual disturbances, headaches and need to be surgically removed when the patient is symptomatic such as in this case.
Bilateral Hand Pain in a Gas Station Worker
Authors: Crystal Estrada, MD., Rabiah Fresco, MD., Bijan Origel, DO., Jesse Cheung, MD., Jay Shah, DO., Abdalhamid Al Harash, MD.
Affiliations: Pomona Valley Hospital Medical Center
Introduction: Hand or other joint pains and swelling can include many broad differentials. Patients can present in any setting, and in our case, avoiding anchoring bias during a Sport Medicine clinic was essential to make a timely diagnosis. An unusual diagnosis of Mixed Connective Tissue Disease (MCTD) may take years to be diagnosed, possibly delaying care and increasing mortality rate. MCTD usually presents with early constitutional symptoms such as fever, fatigue, weight loss, lymphadenopathy, Raynaud phenomenon, myalgias, myositis and may even involve cardiac, renal, nervous, pulmonary or more systems.
Methods: 49 year old female with no past medical history presents to Sports Medicine Clinic with bilateral hand pain and swelling for the past 4 months. She reported persistent pain and swelling around the MCP joints, skin tightness when trying to grip, and episodes of fingers turning blue. Endorsed muscle weakness and weight loss of 10 pounds over 2 months. Denied trauma. Her symptoms were impacting her mobility, daily activities and ability to work at a gas station. There was skin thickening at diffuse hands, feet, distal legs. Salt and pepper rash on left arm. Right hand with diffuse edema and sclerodactyly and synovitis at right PIP joint. Distal fingertips were cool to touch. Upper extremities strength 4 -/4, distally 5/5 and thighs 4/4. No focal deficits. Normal ESR and CRP. Immune work up with + RF, + Sjogren's antibody SSA, + ANA, with further tests +U1 RNP antibodies and the patient was diagnosed with MCTD. She is undergoing treatment with steroids, rituximab, and mycophenolic acid and is closely followed by Rheumatology and Sports Medicine Clinic. Will require long-term follow up.
Discussion: Mixed Connective Tissue Disease is an autoimmune disease that may take years before enough overlapping features commonly seen in SLE, systemic sclerosis, RA, polymyositis, have appeared to be confident that MCTD is appropriate. Diagnosis is met with positive anti-U1 RNP antibodies and at least 3 clinical features such as myositis, acrosclerosis, synovitis, Raynaud phenomenon and digital swelling. It occurs worldwide, affects all races, more common in females, peak incidence in adolescents and in 20s. Estimate annual incidence is 1.9 per 100,000 adults. Mortality estimate is 28% at 10 years. The importance of this case is a lesson in not anchoring. Doing more tests earlier, when the pattern fits an autoimmune diagnosis, since this disease has a high mortality rate.
The Utilization of Osteopathic Manipulative Medicine (OMM) In the Treatment of Migraine Headaches
Authors: Debbie Meskin, DO
Affiliations: Department of Family Medicine at Kaiser Permanente Los Angeles
Introduction: Migraine headaches can be a debilitating condition that affects more than 10% of the worldwide population. There are many effective treatments available, however, each therapy has their own complications and side effects, some requiring management of a specialist. This case study follows a 48 year old female whose migraines have been refractory to most treatments, but had almost complete resolution of symptoms after Osteopathic Manipulative Medicine (OMM), a non-pharmacologic and non-invasive alternative or adjunct to migraine treatment that was performed in a Family Medicine clinic.
Methods: Patient is a 48 year old female with chronic migraine with auras (photophobia) for 21 years. Migraines have been evaluated by Neurology and PM&R specialists and were refractory to four abortive medications, ibuprofen, Cymbalta, nortriptyline, Botox injections, occipital injections, and acupuncture. On initial presentation, patient stated she required both Sumatriptan and Naratriptan daily to relieve symptoms enough to complete her work. Patient was evaluated with the lights off due to her symptoms. Exam revealed hypertonic trapezius and scalene muscles and therefore patient was scheduled for OMM treatment. Patient received trapezius trigger point injections along with OMM treatment that included facilitated positional release, counterstrain, muscle energy, and myofascial release. At preceding visits, patient reported marked improvement of symptoms, and therefore has completed 3 additional OMM treatments. Since receiving OMM treatment, patient only requires Naratriptan for her migraines less than once a week and her prescription of Sumatriptan was able to be discontinued.
Discussion: This supports the use of OMM as a safe and noninvasive alternative or adjunct to treatment of migraine with aura. The OMM techniques performed were low velocity and therefore have few contraindications or complications. There are studies highlighting efficacy of OMM treatment with tension headaches, but less with migraines, making this case unique. Further studies with a larger sample size should be performed to evaluate the efficacy of this treatment, as well as studies identifying which OMM treatment is most successful. However, OMM is a non-pharmacologic and noninvasive treatment performed in an outpatient office that can give patients who have contraindications to pharmacologic treatments or lack of contact with specialists’ access to effective treatment.
A Rare Case of Corynebacterium Infection in a Patient with Liver Cirrhosis
Authors: Fatima Maqsood, DO, Tristan Copeland, MD, Cesar Aguilar Martinez, MD, Nathan McLaughlin, MD
Affiliations: Riverside University Health System/UC Riverside Family Medicine Residency Program
Introduction: Corynebacterium is normal flora present on human skin and mucous membranes. As such, it is often regarded as a contaminant when cultured from blood. However, in immunocompromised patients or those who are otherwise critically ill, it can present as an opportunistic pathogen. Here we present a rare case of disseminated Corynebacterium infection in a 68-year-old female with decompensated NASH cirrhosis.
Methods: A 68-year-old female with past medical history of NASH liver cirrhosis and morbid obesity presented to the ED with abdominal pain, fevers, tachycardia, and shortness of breath. She was admitted for sepsis and acute hypoxic respiratory secondary to a right sided pleural effusion in the setting of decompensated cirrhosis. A diagnostic paracentesis was done in the ED at the time of admission with a SAAG greater than 1.1 and an ascitic neutrophil count of 35. Both sets of blood cultures and ascites fluid cultures all obtained at the time of admission grew Corynebacterium. Patient was started on IV antibiotics to treat Corynebacterium bacteremia with concern for SBP source. During the course of her admission, patient was also found to have a left medial thigh abscess. An I&D of the abscess was performed with subsequent wound cultures growing Corynebacterium. She was ultimately transitioned to oral doxycycline to be continued indefinitely for SBP prophylaxis.
Discussion: Corynebacterium bacteremia is rare. Spontaneous bacterial peritonitis caused by Corynebacterium is rarer still. Often regarded as a contaminant, it presented in this case as an opportunistic pathogen. Multiple factors, including cirrhosis associated immune dysfunction and increased intestinal permeability, put patients with cirrhosis at higher risk of bacterial translocation. For such patients, decompensated cirrhosis with significant fluid overload can present a challenge to successfully treating the infection and preventing re-infection. Transjugular portosystemic shunt (TIPS) placement can be warranted for ascites control. However, in patients who are not a candidate for a TIPS procedure, indefinite prophylactic antibiotics are indicated until better ascites control is obtained.
From Sideline to Strongline: Tackling Foot Pain in a Collegiate Football Player
Authors: Frances Leung, MD, MPH; Bernadette Pendergraph, MD
Affiliations: Harbor-UCLA/Team to Win/Kaiser Permanente Sports Medicine Fellowship
Introduction: Lisfranc injuries are subtle but can have significant long-term consequences if missed. A 19-year-old collegiate football player presented with acute midfoot pain and inability to bear weight following an in-game fall. Initial radiographs were unremarkable, leading to conservative management. However, persistent pain raised concern. This case illustrates the importance of clinical suspicion and advanced imaging in identifying complex injuries that may be underestimated at first glance.
Methods: A 19-year-old football player fell backward during a game with his left foot planted, resulting in immediate midfoot pain and inability to bear weight. At urgent care, exam revealed swelling, ecchymosis, and tenderness over the midfoot, but X-rays showed no fracture or dislocation. He was treated conservatively with NSAIDs, crutches, and a CAM boot. At a 10-day follow-up, symptoms persisted with limited motion. Weight-bearing radiographs showed minimal widening of the Lisfranc interval on the left compared to the right. MRI revealed high T2 signal in the Lisfranc ligament complex. CT showed widening between the 1st and 2nd metatarsals (3.4 mm vs. 2.5 mm, a 36% increase) and between the medial cuneiform and 2nd metatarsal (2.8 mm vs. 1.0 mm, a 180% increase), confirming ligamentous Lisfranc injury. He continued nonoperative care, redshirted the season, and regained full function through rehab.
Discussion: Lisfranc injuries are easily missed, particularly when initial X-rays are normal and pain is nonspecific. This case reinforces the need for ongoing assessment when symptoms persist despite conservative care. In family medicine and sports settings, clinicians must maintain a high index of suspicion for midfoot injuries when patients cannot bear weight or demonstrate localized tenderness. Advanced imaging plays a vital role in clarifying diagnosis and guiding management. Early recognition and appropriate offloading can prevent complications like midfoot collapse and post-traumatic arthritis, especially in young, active patients.
Atypical Presentation of Guillain-Barré Syndrome in an Adolescent
Authors: Gabrielle Marques, DO; Cindy Yang, MD
Affiliations: Department of Family Medicine at Dignity Health Northridge Hospital Medical Center
Introduction: This report presents a case of Guillain-Barré Syndrome (GBS) in a 16-year-old male who initially exhibited muscle and joint pain, fever, headache, nausea, vomiting, shortness of breath, and balance issues. Progressive paralysis developed later, though lower extremity reflexes were preserved. GBS is an immune-mediated polyneuropathy often triggered by a preceding infection, typically marked by symmetric limb weakness and areflexia. Atypical GBS presentations pose diagnostic challenges and may result in delays in treatment.
Methods: The patient presented with bilateral lower extremity weakness, numbness, and slurred speech. Initial workup included a lumbar puncture, revealing elevated cerebrospinal fluid (CSF) protein at 68 mg/dL, while other tests, including meningitis encephalitis panel, inflammatory markers, CSF culture and gram stain, CT and MRI of the brain, chest X-ray, and Electrocardiogram, were negative. There was suspicion of a behavioral/psychiatric component as the patient’s weakness was distractible and he suffered from anxiety and depression. Neurology was consulted and on exam, the patient was unable to lift his extremities against gravity and unable to ambulate more than 12 feet, though reflexes remained intact. His respiratory condition progressively worsened, and he was intubated for airway protection. The patient was transferred to a higher-level care facility, where a second lumbar puncture revealed a protein level of 487 mg/dL. Intravenous immunoglobulin (IVIG) treatment was initiated for atypical GBS, resulting in clinical improvement.
Discussion: Guillain-Barré Syndrome (GBS) and its variants present a growing concern for clinicians due to their diverse and often atypical clinical manifestations. In this case, albuminocytological dissociation was observed, but typical sensory involvement and reflex changes were absent, complicating the diagnosis. The wide variety of GBS presentations challenges clinicians to distinguish it from other conditions with similar symptoms, emphasizing the need for early, accurate diagnosis to prevent severe complications such as respiratory failure. Management generally includes intravenous immunoglobulin (IVIG), with close monitoring of respiratory and cardiac status.Comprehensive outpatient follow-up and rehabilitation for patients with residual deficits often lead to substantial recovery.
Breathless: The Consequences of Delayed Care in Pulmonary Kaposi Sarcoma
Authors: Sasha Haddad, D.O.; Rahul Ahuja, D.O.
Affiliations: Department of Family Medicine at Dignity Health, Northridge, CA
Introduction: Despite significant advancements in antiretroviral therapy (ART), Kaposi sarcoma continues to pose a serious threat to individuals with untreated or advanced HIV/AIDS. Pulmonary involvement, though rare, can be life-threatening. This report illustrates the consequences of fragmented HIV care and delayed intervention, emphasizing the critical need for early diagnosis and continuous medical engagement in high-risk populations.
Methods: A 46-year-old man with HIV/AIDS presented with progressive dyspnea, hemoptysis, fatigue, and violaceous cutaneous lesions. His history included a prior hospitalization for Pneumocystis Jirovecii pneumonia (PJP) in August 2022 and untreated syphilis, with over a year of lost follow-up. On arrival, he was hypoxic (SpO₂ 83%), improving to 93% with 12L oxygen. Chest radiography showed bilateral multifocal opacities, and dermatologic examination revealed violaceous papules and nodules. Skin biopsy confirmed Kaposi’s sarcoma (KS) with HHV-8. Bronchoscopy revealed extensive endobronchial KS, complicated by active bleeding, requiring intubation and mechanical ventilation. Chemotherapy with paclitaxel and continued ART (Biktarvy) were started. Supportive care addressed hyponatremia, thrombocytopenia, and anemia. After 10 days in intensive care, he was extubated with significant clinical improvement. His HIV viral load remained undetectable, and CD4 count began to recover. He was discharged for rehabilitation and further evaluation of an anal mass.
Discussion: This case underscores the severe impact of delayed HIV care, leading to advanced pulmonary Kaposi sarcoma, a rare malignancy that can be fatal in immunocompromised patients if untreated (Martellotta et al., 2009). Delayed care, driven by stigma, resulted in preventable morbidity, including intubation. Early HIV screening, stigma reduction, and consistent follow-up are vital to prevent such outcomes (Cobucci, 2015). The case highlights the need for multidisciplinary collaboration across oncology, infectious disease, pulmonology, and supportive care. Expanding outreach and adherence programs is essential to improving survival in high-risk populations (Engsig, 2014). This patient’s progression, influenced by care barriers, could have been mitigated with earlier diagnosis and treatment.
Lectern Session 2 (3:05 – 3:50PM)
-
Authors: Maxime Rappaport, MD, Rae Godwin, DO, Christopher Kuhlman, MD
Affiliations: Dignity Health Family Medicine Residency at Northridge
Introduction: In 2024, 66% of physicians surveyed by the AMA reported using artificial intelligence (AI) for healthcare. However, AI adoption among resident physicians, particularly in Family Medicine (FM) - where broad clinical knowledge is essential - remains underexplored. While AI has the potential to enhance clinical workflows, unstructured reliance on AI has the potential to impact both residency learning and patient care. We surveyed FM resident physicians about their AI usage, perceptions and residency program policies to inform curriculum development and guide the responsible adoption of AI in medical residency.
Methods: A research proposal was approved by the CommonSpirit IRB as EXEMPT Human Subjects Research. A 29-item Redcap survey was distributed to the program directors and coordinators of 803 Family Medicine residencies in the United States, who were asked to share it with the resident physicians in their programs. Demographics collected including year of birth, state of residency, year in training, and self-perceived proficiency with technology. Data on AI usage frequency, types of tools used, impressions of AI, and current residency policies on AI were gathered. Quantitative data were presented graphically, and open-ended responses were selectively highlighted.
Results: Seventy Family Medicine residents from 23 states responded to the survey. 76% of respondents reported using AI tools in residency, with 44% using them multiple times per day. Residents believed AI enhanced clinical efficiency (71%), medical management (60%), and medical knowledge (61%). Of the 24% of residents not using AI, 59% cited lack of access as the primary barrier. Only 14% of respondents indicated that their residency program provided AI training. 84% expressed interest in training on how to evaluate AI outputs for accuracy.
Conclusion: Family Medicine residents are indeed frequently using artificial intelligence throughout their residency training, with many reporting improvements in clinical efficacy. However, few residency programs offer training on selecting, using, and evaluating AI tools. These survey findings highlight the need for curriculum development that educates residents on how AI works, how to evaluate its outputs, and how to apply the technology to enhance both medical education and patient care.
-
Authors: Amanda Tran, MD, Anita Wong, MD
Affiliations: University of California, Los Angeles Department of Family Medicine
Introduction: Dental caries is the most common chronic childhood disease. One proven therapy to prevent caries is the application of fluoride varnish. Thus, the USPSTF recommends applying fluoride varnish to the primary teeth of all children, and Medicaid programs are required to cover fluoride varnish in primary care settings. Nevertheless, caries remains more prevalent among low socioeconomic and minority groups. Therefore, the aim of this QI project is to increase documentation and delivery of fluoride varnish among children at the resident clinic at the Mid-Valley Comprehensive Health Center, which serves low-income and Hispanic populations.
Methods: A pre-intervention chart review of 6-month to 5-year-old Well Child Checks (WCC) was performed over a 3-month period (10/1/2024-12/31/2024, n=23). The following variables were collected: (1) the documentation of the fluoride varnish need or lack thereof, (2) the application of varnish during a WCC if needed, and (3) the reason why no varnish was applied if needed. The intervention consisted of a WCC note template that incorporated documentation of the above variables and an order set to have medical assistants apply varnish at the end of a WCC. A post-intervention chart review was conducted over a 3-month period (1/1/2025-3/31/2025, n=29). A chi-squared test with alpha=0.05 was used to determine statistical significance between pre- and post-intervention periods.
Results: In the pre-intervention period, fluoride varnish was given to 10% (1/10) of eligible patients. Reasons why varnish was not given to eligible patients included deferral to a dentist (45%), followed by time constraints (11%) and parental declination (11%). There was no explanation for the omission in 33% of eligible patients. In the post-intervention period, fluoride varnish was given to 50% (7/14) of eligible patients. Reasons why varnish was not given to eligible patients included deferral to a dentist (72%), followed by time constraints (14%) and parental declination (14%). There was a significant difference between pre- and post-intervention varnish application rates [chi-square (1, N=24) = 4.2, p=0.04] but not documentation rates [chi-square (1, N=51) = 1.1, p=0.29].
Conclusion: Implementation of a WCC note template and fluoride varnish order set significantly increased varnish application rates. This finding suggests that standardized note templates with visual reminders and order sets that streamline workflows can improve practices. Furthermore, the high percentage of eligible patients who did not receive varnish due to deferral to a dentist highlights a missed opportunity in primary care settings. Since children often see PCPs more than dentists, integrating varnish application into WCCs can increase access to dental services and reduce disparities in oral health.
-
Authors: Angela Deng, MD (1), Olayemi Osibowale, MD (1), Anthony Bao, PharmD (2), Monique George, MD (1), Hasmig Ekmekdjian, Pharm.D., APh (2), Kimi Pontoppidan, Pharm.D., APh (2), Annette Adams, PhD, MPH (3)
Affiliations: (1) Department of Family Medicine at Kaiser Woodland Hills; (2) Department of Pharmacy at Kaiser Woodland Hills; (3) Division of Epidemiologic Research at KPSCAL
Introduction: Guidelines for the treatment and monitoring of osteoporosis and osteopenia recommend specific durations for bisphosphonate (BP) therapy and ongoing monitoring for disease progression. However, real-world adherence to these guidelines is not well characterized. This study examines whether practices at Kaiser Permanente Southern California (KPSC) align with these guidelines by addressing two key questions: (1) Is the total duration of BP therapy consistent with guidelines? (2) Are DXA studies ordered or completed within the recommended time interval after starting oral bisphosphonates?
Methods: Retrospective cohort study analyzing female KPSC members aged ≥50 years with osteoporosis/osteopenia or a prior hip fracture who received ≥2 oral BP dispenses from 1/1/07–11/31/18. Data was extracted from KPSC outpatient pharmacy dispense data and electronic health record. Primary outcomes were: a) adherence to BP for 5-9 years, with discontinuation after 10 years, b) completion of DXA scans after starting and after discontinuing BP. Secondary outcomes were major osteoporosis-related fractures (MOF), identified with ICD-9/ICD-10 codes. Cohort characteristics and outcomes were quantified as median and interquartile range (IQR) for continuous data and as numbers and proportions for categorical data.
Results: Among the 196,129 women in the cohort, 53.3% were White and 24.0% were Hispanic, with a median age of 67.4 years (IQR 60.2-75.7 years). Median BP therapy duration was 1.8 years (IQR 0.5-4.5), with 16.0% of women persisting for the recommended 5-9 years of treatment and 6.0% continuing beyond 9 years. Among those on BPs for 5-9 years, 12.1% received DXA scans within 2-3 years after bisphosphonate discontinuation. Among those treated for 9+ years, 8,669 patients underwent DXA monitoring following therapy completion. MOF occurred in 20.2% of female patients after bisphosphonate initiation.
Conclusion: The findings highlight that only a small proportion of patients adhered to the recommended bisphosphonate treatment duration, and post-therapy DXA monitoring rates were suboptimal. While a causal relationship has yet to be established, these findings highlight the need for interventions to improve adherence to guidelines and optimize patient outcomes.
-
Authors: Kun Woo Lee, DO, Huy Ho, DO, Venus Esquivel, MD, Molly Kivumbi, MD, Bruce Weng, DO, Esther Zarecki, MD, Nathan McLaughlin, MD
Affiliations: Riverside University Health System
Introduction: Helicobacter pylori (H. Pylori) affects two thirds of the world’s adult population. H. Pylori is a gram negative bacterium linked to multiple gastrointestinal diseases including chronic gastritis, peptic ulcer disease (PUD), and gastric malignancy. Though antibiotics are the mainstay of treatment, increasing antibiotic resistance has led to increased treatment failure. This study looks to document these patterns in Riverside County to help decrease redundant costs due to re-treatment and prolongation of antibiotic exposure.
Methods: A total of 150 patients aged 18+ with positive H. Pylori tests (urea breath test, stool antigen, or EGD biopsy) from January 2019 to April 2022 were included in this retrospective cohort study. The groups were separated into those treated with triple versus quadruple therapy. They were further stratified by age, sex, and gender to evaluate for treatment effectiveness. Inclusion criteria were patients with confirmed H. pylori infection, and exclusion criteria included non-adherence, loss to follow-up, or treatment outside the study period. This retrospective study evaluated treatment outcomes at the Moreno Valley Community health center using EPIC records and RUHS statistics to analyze cure rates after treatment.
Results: Patients were analyzed with intention-to-treat (ITT) and per-protocol (PP) methods, divided into triple and quadruple therapy groups. No randomization was done as it was a retrospective study. Among 150 patients, there were 4 patients who did not complete therapy, and 52 patients excluded due to non-adherence to medications or lost to follow up. Treatment success was defined by negative TOC after full treatment. ITT success rates were 45.3% for triple therapy and 69.8% for quadruple therapy. PP success rates were 82.9% for triple therapy and 95.1% for quadruple therapy. Quadruple therapy had a higher eradication rate, but secondary outcomes showed no significant difference between concomitant and bismuth quadruple therapies.
Conclusion: This retrospective study in Riverside County showed significantly higher cure rates for H. pylori with quadruple therapy compared to triple therapy. No significant difference was found between bismuth and concomitant quadruple therapies. Given increasing antibiotic resistance, quadruple therapy is more effective and should be considered first-line treatment. Effective initial treatment reduces healthcare costs by preventing complications like peptic ulcers and gastric malignancies. Providers should consider local resistance patterns and emphasize treatment adherence for better outcomes.
Thank You
-
The Multi-Campus Research Committee expresses deep appreciation to Dr. Gerardo Moreno and the UCLA Department of Family Medicine for their continued financial support of the Multi-Campus Research Forum.
We are especially grateful to the HRSA-funded UCLA DGSOM Center of Excellence (UCLA COE) for its financial support of this year’s Research Forum.
A huge thank-you to Felicia Winningham for diving in headfirst to assist with administrative management of this year's forum, and Damilola Jolayemi, Uyen Kao, and Enrique Sanchez (from UCLA CHIPTS) for their invaluable assistance with event coordination. We also thank Valencia Moody for her assistance with purchasing matters.
Last, but certainly not least, the Committee is extremely grateful for the administrative direction of Laura W. Sheehan, who has been running this event since she joined UCLA Family Medicine over 12 years ago.

-
We encourage all attendees to please stay for the entirety of this year's event. We will be raffling gift cards (to Target, Amazon, and Starbucks) for three lucky attendees at the very end of Research Day. If you are able to stay until the end of today's event (4pm), please be sure to enter the raffle at the Check-In desk to enter your name into the raffle. You must be present to win!