Scientists at the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA have identified key metabolic mechanisms that squamous cell skin cancers use to resist treatment, offering new insights into how to potentially stop cancer growth.
Their findings, published in Science Advances, highlight the need for combination therapies that target multiple metabolic pathways simultaneously. This approach could lead to more effective therapies not only for squamous cell skin cancer, which forms in cells on the surface of the skin, but also for the myriad other cancers that share similar metabolic hallmarks.
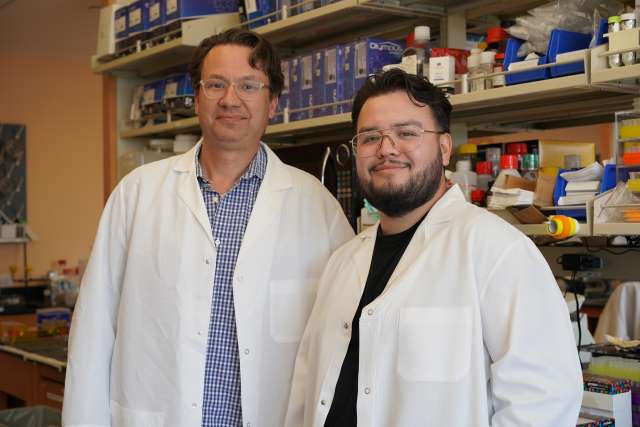
The research was led by senior author William Lowry, a professor of molecular, cell and developmental biology at UCLA.
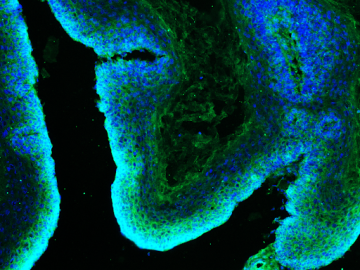
In 2019, Lowry and his colleagues overturned a fundamental doctrine of cancer metabolism theory known as the Warburg effect, which stated that cancer cells primarily rely on glucose for energy. Instead, they found that squamous cell skin cancer cells are metabolically flexible: When glucose is unavailable, they can switch to derive energy from the amino acid glutamine.
“Our data suggest that the reason previous clinical efforts to target cancer metabolism have failed is that they focused on just one pathway at a time,” said Lowry, associate director of education and technology transfer at the UCLA Broad Stem Cell Research Center. “In a living organism, there are multiple nutrients available that tumors can use to fuel their growth, making single-pathway interventions insufficient.”
Building on this work, Carlos Galván, a graduate student in Lowry’s lab and the new study’s first author, has been investigating the extent of this metabolic flexibility and whether it could be curtailed. Working with mouse models, he genetically blocked the pathway glutamine uses to fuel cells in hair follicle stem cells — a known cell type of origin for squamous cell skin cancer — and observed its effect on the formation and growth of tumors. As with the previous experiments, the tumors simply switched to another nutrient source.
“It’s kind of like whack-a-mole,” said Galván, who is also part of the UCLA Broad Stem Cell Research Center Training Program. “When you block one metabolic pathway, the cancer cells are just flexible enough to find another nutrient to fuel their growth.”
Next, the researchers tried what they call a “double hammer” approach: genetically blocking the pathways for both glucose and glutamine metabolism by deleting the transmitter that allows uptake of respective enzymes. This dual-target strategy was enough to prevent the cancer from growing in mouse models.
Galván also sought to identify the mechanisms that enabled the cancer cells to rewire their metabolic programs to continue growing when one nutrient pathway was blocked. Interestingly, he found that the metabolic flexibility was not driven by a transcriptional response, as initially suspected, but by a rapid redistribution of transporter proteins to the cell membrane, allowing the cells to uptake alternative nutrients.
The research team is working on replicating their genetic findings by using pharmacological inhibitors to target the specific enzymes involved in these metabolic processes. To bring this therapeutic strategy to patients, the team is focused on identifying and testing the right combination of drugs that can achieve the same effects observed with genetic manipulation.
Adding another layer of complexity, the researchers are interested in ultimately developing a topical treatment that could be applied directly to the skin. This approach offers a unique advantage: targeting the tumor site specifically, potentially minimizing side effects often seen with oral treatments.
“One advantage of treating skin cancer is the accessibility of the tumor,” Galván said. “Applying the treatment topically, with a gel or lotion, could be more effective and safer than systemic treatments. But we still face challenges, such as ensuring the drug can penetrate the skin barrier and remain potent over time.”
Because various other cancers also use glucose and glutamine to fuel their growth, the study’s implications extend beyond squamous cell skin cancer. The researchers are currently working on applying this strategy to other cancers, such as melanoma.
The researchers are also exploring the protein and post-transcriptional regulation that enables metabolic flexibility.
“If we can figure out how cancer cells sense and respond to metabolic stress, we could potentially target the underlying mechanisms and defeat them in this quest for flexibility,” said Lowry, who is also the co-director of the Education, Training, and Mentoring Program at the UCLA Health Jonsson Comprehensive Cancer Center. “That could be an alternative to just blocking the transporters pharmacologically.”
The experimental drugs mentioned were used in preclinical tests and have not been approved by the Food and Drug Administration for human use.
Other UCLA authors include Aimee Flores, Victoria Cerrillos, Itzetl Avila, Conor Murphy, Wilson Zheng and Heather Christofk.
The study received support from the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the National Cancer Institute.
Galván was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases’ Dermatological Scientist Training Program, the Eli and Edythe Broad Center of Regenerative Medicine at UCLA, the Broad Stem Cell Research Training Program and the Stem Cell Research Rose Hills Foundation Graduate Scholarship.