My plane from New York was landing at LAX when I started to feel a little headachy and had a bit of a sore throat. It was early March, and the COVID-19 pandemic was starting to make its deadly presence known in the United States, starting in Washington State and then appearing on the East Coast. I had been in Manhattan for a conference of emergency physicians when National Guard troops occupied and locked down the city of New Rochelle, about 20 miles to the north, where a cluster of the illness had erupted.
My colleagues and I had been watching, with increasing alarm, the terrible toll of this pandemic as it unfolded faraway in China and Italy, and we wondered what it would be like when it landed on our shores. Now it was here.
I had taken precautions on the plane. I wore a mask and the seat next to me was empty. I spent most of the flight reading what little medical literature there was at the time about SARS-CoV-2. I wasn’t terribly concerned about my relatively minor symptoms; I had been traveling and I was stressed, concerned about my family and what might await me in the hospital. It didn’t occur to me that maybe I was sick with this virus.
I started to feel worse once I got home, but I was supposed to work a shift. I called my medical director in the emergency department (ED) and reported that I felt a little sick, but not terrible, that I had just been in New York, but I didn’t have a fever or a cough. Still, my medical director thought I should get tested. I was positive. I am very lucky, though. My illness wasn’t severe, and I just needed some time at home in bed to recover.
My first shift back was strange. Usually, there is a kind of sizzle in the ED as the staff constantly moves among patients. This day, it was eerily quiet and there were a lot of small conversations taking place among groups of people. It was a very different energy, and there was an undercurrent of fear. That is not something you often feel among the staff in an ED. We are trained to adapt and cope and care for patients in the most difficult situations. But this felt different. Not only was there concern for our patients, there also was concern for ourselves and the potential personal risk we would be facing.
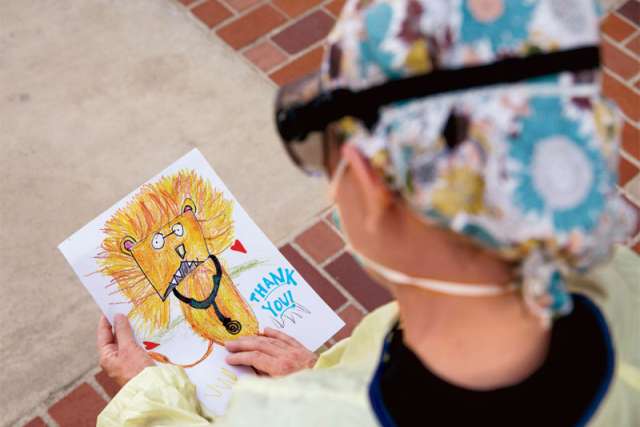
The necessity to wear personal protective equipment (PPE) makes our day-to-day work more difficult. There’s a term for it: PPE fatigue. Even though I’ve already had COVID, I don’t know if I can be re-infected, and I am very vigilant about PPE. Some of us don’t take our N95 masks off for an entire shift, which means we are not able to eat or take in any fluids for at least eight hours. When a patient comes into the ED in urgent need, we can’t just run into the room like we used to. We have to stand outside putting on full PPE — gowns, appropriate masks, eye protection, gloves — as quickly as possible before going in. That cuts against our instinct as frontline emergency caregivers to run toward the fire, toward someone in need.
There was a patient that EMS brought in — she was breathing very quickly and clearly was in distress. As EMS was putting her in one of our negative-pressure rooms and I was putting on my PPE, we made eye contact. She wasn’t talking, but her eyes pleaded “Help me!” I wanted to rush in but I couldn’t; I had to put on my PPE first. A frontline worker in the Ebola epidemic famously said: “There is no emergency in a pandemic.” It is a reminder that we have to protect ourselves so that we can continue to care for our patients. Maybe it takes less than a minute to put everything on, but it feels like an eternity. Any delay in delivering patient care is hard to swallow.
The precautions don’t stop at the end of my shift. That is another piece of this that makes it hard — how my professional life bleeds into my personal life and the concern I have at the end of the day for my family. When I was still sick, my husband and I talked about the best way to decontaminate after I went back to work. I have a ritual when I get home. My shoes come off in the car and I put them in a bin high up in the garage so my kids can’t get to them. I’ve changed into a new set of scrubs before coming home; those come off right at the entrance of the laundry room, and they and my work scrubs and my hair cover and my socks go into the washing machine. Then I go directly into the shower.
One morning, I arrived for my shift, and there was a man who had been brought in during the night with a medical condition from which he was unlikely to recover. He had been stabilized, but no one from his family was there to talk with about a plan for his care. We were about to send the patient to the ICU, when the family pulled up in their car outside the ED. I went out in my PPE to talk with them.
The sun was rising and cast a soft morning light. There I was, outfitted head to toe in protective gear, having a muffled conversation through my N95 mask and face shield about end-oflife care with a distressed family huddled inside their car in the parking lot. At any other time, this would have been a typical conversation with the family of a critically ill patient. I would have sat close, reached out, hugged them. I would have made human contact. But on this day, in this pace, under these circumstances, there was none of that — no hugs, no contact, no human touch. Just heartbreak and the professional ache of having to have this difficult conversation with a grieving family while standing in a parking lot wrapped inside a protective cocoon.
No, it was not typical. Like most everything else since this pandemic began, it was surreal.