As director of UCLA’s new Goodman-Luskin Microbiome Center, Elaine Hsiao, PhD, leads groundbreaking research into how our resident microbes help regulate human health.
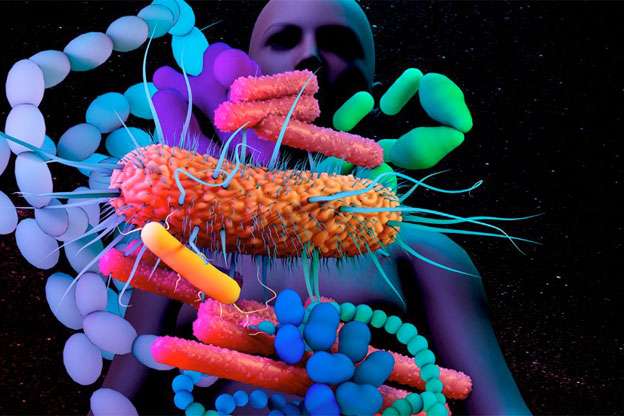
One of the most buzzed-about areas of biomedical research is the study of the human microbiome — the population of bacteria, viruses and fungi that inhabit our bodies — and its impact on our physical and mental well-being. Elaine Hsiao, PhD, De Logi Professor of Biological Sciences, is an up-andcoming leader of this emerging field. Since launching her lab in 2015, Dr. Hsiao has published a raft of groundbreaking papers on the relationship between the gut microbiome and the brain and how it influences processes ranging from neurodevelopment in fetuses to neurotransmitter production in adults. In 2022, she was one of three researchers to be honored by the New York Academy of Sciences with a Blavatnik National Award for Young Scientists. This past February, she was named founding director of UCLA’s Goodman-Luskin Microbiome Center, established with a $20 million gift from Andrea and Donald Goodman and Renee and Meyer Luskin. She spoke with contributing writer Kenneth Miller about the wonders of the microbiome and her vision for the center.
Interest in the microbiome seems to have skyrocketed in the past decade. Why is that?
Dr. Hsiao: In part, it’s because we’re just beginning to grasp the topic’s importance. Before the advent of genetic -sequencing technologies, it was very hard to study these microbial populations. In 2012, the Human Microbiome Project gave us the first snapshot of the different bacteria living in a healthy human body. Yet, there’s still so much to learn. We don’t know what constitutes a healthy microbiome versus an unhealthy one; to some extent, it seems to vary according to the individual. We also don’t know much about the non-bacterial members of the population. This is such a vast and complex group of microorganisms! They outnumber human cells 10-to-one, but they’re so small that they make up only 1% to 3% of our body mass. The largest numbers are in the gastrointestinal tract, where there are 100 trillion bacteria alone, but they’re plentiful in other places as well — the skin, the eyes, the reproductive tract. What’s become increasingly clear, though, is that they play many crucial roles across different organ systems.
How do these microbes interact with our bodies and brains?
Dr. Hsiao: They produce a lot of metabolites, or signaling molecules. These organisms can communicate with neurons and plug into sensory signaling pathways. They interface between our cells and the foods we eat, the medications we take, the environmental exposures we encounter. They interact with our immune system, our hormones, our metabolism. They affect both our risk of disease and our response to drugs that are used to treat disease.
Can you share some examples of the influence they exert?
Dr. Hsiao: My own team’s research centers on the gut-brain connection. In one study, we discovered that metabolites produced by the gut microbiome of pregnant mice can influence fetal neurodevelopment, with lasting effects on the behavior of their offspring. Mice born to mothers with depleted microbiomes had reduced white matter in their brains and an impaired sense of touch. In another study, we found that certain gut bacteria regulate levels of the neurotransmitter serotonin and interact with common antidepressants, such as selective serotonin reuptake inhibitors, or SSRIs. And in a third study, we found that changes in the microbiome explain why eating a low-carbohydrate, high-fat ketogenic diet helps control seizure disorders; in mice, the regimen changes the proportions of bacterial species that affect levels of the neurotransmitter GABA. We think these sorts of gut-brain interactions can impact a whole range of neurological disorders — things like depression, Parkinson’s, autism spectrum disorder and Alzheimer’s disease. There’s also some evidence that the microbiome can influence the protein misfolding and aggregation that are seen in Alzheimer’s and some other neurodegenerative disorders.
All of this seems to suggest that the microbiome can directly influence behavior.
Dr. Hsiao: Absolutely. Across a bunch of lab animals — like mice and rats and zebrafish and flies — we’ve found that if you manipulate the microbiome, they start behaving differently. And if you change their microbiome to resemble that of an animal with a neurological disease, they’ll behave as if they have that disease. More and more studies are also showing that the microbiome is also involved in behavioral problems like eating disorders and addiction. The reasons aren’t clear yet, but the correlations are intriguing.
That’s kind of spooky. So, are we at the mercy of these microbes’ whims?
Dr. Hsiao: Well, it’s a two-way street. The microbiome can also be altered by our diets, our stress levels, the amount of sleep we get, habits like smoking and alcohol use, and other behaviors. We’re still working out questions of causality — in many cases, a kind of feedback loop may connect the microbiome’s behavior and our own.
Has microbiome research led to any effective therapies?
Dr. Hsiao: The FDA approved the first microbiome-based therapy just last December — an enema based on a defined community of microbes to treat the intestinal infection Clostridioides difficile. Fecal transplants have already been used experimentally for several years to treat C. difficile, with high success rates. Based partly on our findings around the ketogenic diet and seizures, researchers are now testing probiotics for refractory epilepsy. Several other types of probiotics seem to be beneficial for other ailments, though there’s little evidence that commercially available products work as advertised. But we think these treatments are just scratching the surface of what microbiome-based therapies could eventually do. The hope is that the microbiome can be leveraged for a wide range of interventions. Specific microbes or their metabolites could be administered to patients in oral pills as treatments for specific diseases. The composition of a patient’s microbiome could serve as a biomarker to enhance the efficacy of existing drugs — say, to guide selection of chemotherapy agents for patients with different proportions of gut microbiota — or to detect disease or an individual’s risk of disease.
How will the new center advance microbiome research at UCLA?
Dr. Hsiao: Our goal is to provide a collaborative ecosystem for microbiome research that will propel new discoveries, leading to improved clinical care. We’re hoping that the center will unite people across the UCLA campus — not just the school of medicine, but also life sciences, the physical sciences, engineering, anyone with microbiome- research interests. That includes researchers who maybe don’t have the expertise to run some of the core techniques required and could benefit from working with those who do. We’re pursuing several different areas of focus, including cardiovascular disease and lipid metabolism, inflammatory bowel diseases, liver disease, mental illness and pain, neurodevelopmental and neurodegenerative diseases, obesity and metabolic disorders and substance use disorder. We’ll be investigating the role of the microbiome in all these conditions, and researching therapeutic approaches based on those disease pathways.
What kind of infrastructure will the center provide for that work?
Dr. Hsiao: We’re launching a number of core facilities, which we hope will draw new talent into the field. We’ll have a microbiome-sequencing facility. We’re starting a gnotobiotic animal facility, where you can raise animals completely germ-free — that is, with no microbiome — and start colonizing them with microbial communities that you’re interested in. There’s already a biostatistics and informatics core. With microbiomes being so enormous and complex, you generate huge data sets, and you need sophisticated ways of integrating them. We’ve also got a neuroimaging core to help us visualize how changes in the microbiome affect the brain.
What excites you most about this project?
Dr. Hsiao: I graduated from UCLA with a BS in microbiology, immunology and molecular genetics. This is where I first learned to love molecular biology and microbes. I came back eight years ago to work with the outstanding group of scientists here who specialize in gut-brain and brain-gut interactions. The Goodman-Luskin Microbiome Center gives us the opportunity to span the entire range of microbiome science, from the most fundamental basic research to the most impactful translational research. I’m confident that in the next few years, we’ll be able to push the boundaries forward and show how gut microbes influence chronic diseases that extend far beyond the GI tract, affecting not only the brain, but also organs like the heart and liver. It’s such an amazing time to be in this field. I’m thrilled to have the chance to explore new frontiers and make breakthroughs that will ultimately benefit people around the world.
For more information about the Goodman-Luskin Microbiome Center
