
The ‘bionic possibilities’ of prosthetic advances
Step into the lab of Tyler R. Clites, PhD, on the second floor of the UCLA Health Outpatient Rehabilitation Services building, and you enter a world of the bionic future — a time when advanced surgical techniques and precision-engineered prosthetic limbs will provide full functionality and sensation without pain and joint replacements will last a lifetime.
Showing a visitor around the lab, Dr. Clites, assistant professor of mechanical and aerospace engineering at UCLA’s Henry Samueli School of Engineering and Applied Sciences and orthopaedic surgery at the David Geffen School of Medicine at UCLA, opens a door with a sign ominously warning “Biohazard.” “This,” he says, “is the KUKA Room.”
The KUKA — a brutish orange industrial robot with a hefty articulated arm — stands in the room’s center. Typically used on an auto-assembly line, the KUKA in Dr. Clites’ lab has been reprogrammed to test the effect of various forces on the joints of cadaveric human body parts — arms, thumbs, knees, ankles — as well as on an array of prosthetic devices. “It can produce enough force to rip a knee apart or tear an ACL,” Dr. Clites says. “That’s what we use it for.”

Next door, the Surgical Innovation Suite and an adjoining Biomechanics Room complete this warren of creativity, a multidisciplinary space where UCLA bioengineers, orthopaedic surgeons and medical and graduate engineering students work together to imagine and develop new prosthetic devices and implants. Since arriving at UCLA a few months into the COVID-19 pandemic, Dr. Clites has forged collaborations with a dozen orthopaedic surgeons on nine projects. These include ankle and thumb implants, a novel attachment using an electromagnet for leg and arm prostheses and an implant to prevent anterior cruciate ligament (ACL) injuries.
It is a field blending engineering and medical science that Dr. Clites has dubbed “anatomics.” As described on the website for Dr. Clites’ Anatomical Engineering Group, anatomics explores the “bionic possibilities at the intersection of innovative surgery and advanced robotics.” It envisions a future in which, Dr. Clites says, “efforts of surgeons and mechatronic engineers [who combine mechanics, electronics and computing] are synchronized in the co-development of body and machine in pursuit of bionic performance that is superior to what is possible with mechatronics alone.”
“This is no longer the stuff of science fiction,” Dr. Clites says. “Already, humanity has built incredible exoskeletons and prostheses that restore locomotion to persons with physical disability, and even augment able-bodied performance. By combining surgical and mechanical design to co-engineer body and machine, our long-term goal is to transform the field of human rehabilitation and augmentation by making anatomics a fundamental tenet of bionic development.”
It is, says orthopaedic and plastic surgeon Kodi Azari, MD (FEL ’04), chief of reconstructive transplantation, and one of Dr. Clites’ surgical collaborators, an exciting and hopeful future. “The technology is advancing at such a pace that now we can become really creative and try to think about what we can do to get a person as close as possible to where they were before the loss,” he says.

Back in the Kuka Room, Dr. Clites holds a broken black-plastic prototype of a 3D-printed device that was imagined to replace the function of the talus bone in the ankle. Breaking the talus, a small bone located between the lower leg bones and the heel that has a critical role in supporting a person’s weight and movement, is a serious injury, and patients often face a difficult choice: either fuse the bones and limit functional mobility or amputate the foot. Dr. Clites and Nelson F. SooHoo, MD (FEL ’02), a specialist in foot and ankle surgery, have been collaborating on this “compliant” support device — a flexible mechanism that closely mimics the motions of the natural world by bending rather than rubbing, sliding or rolling. They hope their device will not only save the limb, but also, because it is frictionless and does not wear, last a patient’s lifespan.
But first, it must be tested.
“We push them to failure,” Dr. Clites says of the prototypes that are arrayed around the KUKA Room. “They’re supposed to fail. The question is when do they fail, and how.”
Through their failures and successes, Dr. Clites and his UCLA Health collaborators foresee a new era in prostheses and implants, a time in which amputations are no longer considered failures. Rather, they are performed with exquisite care to preserve nerves, muscles, function and sensation as engineers like Dr. Clites develop advanced prostheses “with the patient in mind, leveraging new body structures to create the next generation of bionic technologies.”
“These patients are complex, amazing, incredible human beings, with deeply held passions and hopes and dreams,” Dr. Clites says. “We’re trying to help them have access to whatever they want by tearing down some of the barriers that exist systemically around them.”
Nicholas M. Bernthal, MD (RES ’12), chair and executive medical director of the Department of Orthopaedic Surgery, is one of the UCLA Health surgeons working closely with Dr. Clites to improve outcomes for patients who have undergone an amputation. “He is every surgeon’s dream,” Dr. Bernthal says of Dr. Clites. “He is a guy who wants to solve problems.”
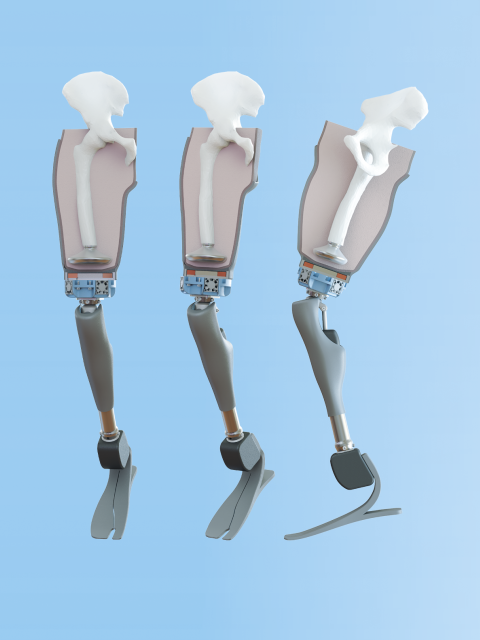
Dr. Bernthal and Dr. Clites, as well as Alexandra I. Stavrakis, MD ’10 (RES ’16), an orthopaedic surgeon specializing in the hip and knee, have been working to improve how prostheses attach to the body. “One of the big issues following amputation is the socket pulling on the stump,” Dr. Bernthal explains. “The socket squeezes all of the tissue between the socket and the bone. That creates a pistoning motion, back and forth and up and down with every step. That’s a very painful experience over the course of a million steps a year.”
Together, the investigators theorized that implanting a piece of steel coated with titanium nitrate in the residual stump and placing an electromagnet in the socket of the prosthesis would improve both fit and control. With a pair of grants from the National Science Foundation and the U.S. Department of Defense totaling $1 million, they developed such a device. “The goal is to have the energy expenditure of walking with a prosthesis be no more than walking without an amputation,” Dr. Bernthal says.
Development of the device did not come without its own friction. “He [Dr. Clites] wants the magnet to be as big as possible,” Dr. Bernthal says. “The stronger the magnet, the more he can do with it. That’s an engineer’s perspective. A surgeon’s perspective, on the other hand, is that I need the magnet as small as possible. If it irritates the soft tissue, that’s a non-starter.”
The magic of such collaborations, Dr. Clites says, “is that we seek out a sweet spot within this tension where this solution can have the most impact.”
“WE PUSH THEM TO FAILURE. THEY’RE SUPPOSED TO FAIL. THE QUESTION IS WHEN DO THEY FAIL, AND HOW.”
In the lab, the researchers use motion-capture cameras to track the movement of their designs in 3D space. The results lead to further adjustments and new design iterations that are followed by more testing, all contributing to the unfolding evolution of the device. “The joy of working collaboratively together on something like this,” Dr. Bernthal says, “is being able to sit down, draw something on a piece of paper and take it all the way to a human clinical trial and improve the lives of patients.”
An important focus for Dr. Clites is to make the promise of anatomics accessible to the broadest-possible population of patients. As the equity, diversity and inclusion officer for his department in the Samueli School, he is keenly aware of past inequities that have prevented many patients — particularly those from underrepresented and underserved communities — from accessing appropriate care.
As an example, he notes that “a Black person with diabetes in the U.S. is four times as likely to have an amputation as a white person. That is a staggering disparity. There is nothing inherent to race to explain it; it’s about access to food and appropriate medical care,” he says.
“Awareness of issues around diversity, equity and inclusion must permeate all the research that we do. If I’m building a new prosthetic device, and I know that diabetic amputation is the most common type of amputation, but that it also is more likely to affect Black Americans than white Americans, then I must make sure that anything I design is going to be accessible to people with diabetic amputations,” Dr. Clites says. “The people least likely to be able to afford this care are the same folks who are most likely to need it, and that has to be at the forefront of our thinking when we are designing these devices.”
Following an amputation, prosthetic care and socket fitting is time and resource intensive, and patients can incur thousands of dollars in out-of-pocket expenses. “Often, the socket has to be replaced or remade because people’s limbs change shape and size. If a patient can’t afford it, they run what may be an even more profound risk of developing skin lesions that can knock them off their feet, which itself can further exacerbate the financial strain, or even lead to further amputation,” Dr. Clites says.
“To make a device that targets issues in post-amputation care, my focus needs to be on improving socket fit and reducing the need for adjustment in the clinic, because those are costly issues currently affecting people in underresourced communities. If we can design a device that is adaptive to changes in limb shape and size — which our magnetic-attachment approach does — then a lot of that cost can be avoided. Understanding these factors is essential in developing technology that will benefit underserved populations.”

The earliest-known prosthesis is a wooden big toe, attached with leather straps to the body of a mummified Egyptian noblewoman. It dates back 3,000 years. Centuries later, prosthetic limbs made from wood and metal were found amid the remnants of the Roman Empire and the Middle Ages. Although Ahab, the fictional captain of the Pequod that Herman Melville wrote of in Moby-Dick, sported a prosthetic leg fashioned from a whale bone, the standard prosthesis of the mid-1800s was a peg carved from wood.
Needless to say, the field has evolved. Battlefield injuries from two world wars in the 20th century spurred accelerated development of artificial limbs, and increased interest from the defense department further speeded up work in functional prostheses.
But it was not until the turn of the current century that work in the field really exploded, with an array of futuristic (at the time) devices: implanted biocompatible electrodes, osseointegrated implants embedded directly into the bone, robotic prosthetic limbs and devices controlled by signals emitted from muscles and nerves. “It’s a great time to be in the field,” Dr. Clites says. “All of these pieces were developed in isolation and are now being integrated into full-stack bionic systems.”
However, for a patient to fully benefit from these bionic systems, surgical techniques for amputation must progress, as well. While techniques have advanced to the point that the majority of damaged limbs can now be salvaged rather than amputated, results for the remaining patients for whom amputation is the treatment of last resort can be less than optimal, often leaving patients with painful neuromas and phantom limb pain. “A patient is giving up a limb for some reason — a blast wound, cancer, a crushing injury — and in return we must bring every bit of our best intellectual and engineering and surgical brainpower and knowhow to enable them to get back to a normal life,” Dr. Bernthal says.
Amputation, Dr. Clites adds, “should not be seen as a clinical failure, but instead as another type of limb-salvage procedure.”
In 2021, Dr. Clites published a paper in which he and his co-authors urge the medical community to adopt new techniques such as targeted muscle/sensory reinnervation (TMR) and regenerative peripheral nerve interface (RPNI) as standard of care.
At UCLA Health, orthopaedic surgeon Lauren E. Wessel, MD (FEL ’22), and plastic and reconstructive surgeon Michael R. DeLong, MD (RES ’21), have established a specialized clinic to standardize these procedures. “Amputee care is complex, both from a psycho-social perspective and from a reconstructive perspective,” Dr. Wessel says. “Neuropathic pain after amputation has been well documented in this population and has not been adequately addressed. By using surgical techniques like TMR and RPNI, we can reduce the amount of opioid medication a patient must take to control their pain by about 80%.”
While visiting other centers that routinely use TMR and RPNI, Dr. DeLong has noted that patients experience lower pain levels, and a higher percentage successfully ambulate after surgery. “Some of these novel techniques have only been publicized in the last decade,” he says. “It takes a generation for them to be adopted at new sites, but this should be considered standard of care.”

At the start of a new collaboration, Dr. Clites often begins with a simple question: What is a problem you have that can’t be solved?
After some brainstorming, the surgeons and engineers test their ideas in the Surgical Innovation Suite, which is equipped with a surgical table, drawers filled with instruments, PPE and a freezer holding parts of cadavers. The only thing missing from making it a full operating room, Dr. Clites says, are monitors and their accompanying beeping.
With the surgeon on one side of the table with a scalpel and medical and engineering students on the other, they begin the process. “Can we pick this muscle up and put it here?” Dr. Clites says. “Can we move this bone here? How much space can we create? It’s like we’re debugging code. You need to have that code open in front of you and work through it. It is hard to do in the abstract.”
Dr. Azari has been at that table. His specialty is the hand — in 2011, he led a team of surgeons to perform the first hand transplant at UCLA Health — and he notes that development of the opposable thumb 2 million years ago played a significant role in shaping human evolution by allowing humans to manipulate objects. If someone loses their thumb, they lose 40% of their hand function.
Dr. Azari and Dr. Wessel, also a specialist in hand surgery, are partnering with Dr. Clites to develop a thumb implant to help patients regain full function. Their idea is to cover the implant with skin and subcutaneous tissue from the forearm to provide functionality and sensation. “You would attach [the skin flap] to the nerves at the cut end of the thumb, where they can grow into each other and innervate the implant,” Dr. Azari explains.
Sachi Bansal, a doctoral student in bioengineering who is working on the thumb project, is doing initial test-of-concept work on rats to see how well the skin adheres to the implant, and to devise ways to improve it. “I’m excited about the potential,” she says.
Dr. Wessel studied civil engineering as an undergraduate student and is deeply interested in device design. “It’s nice to have a collaborator who really treats you as a teammate,” she says of Dr. Clites.
“Dr. Clites is an engineer who thinks he’s a surgeon masquerading as an engineer,” Dr. Azari adds. “There are certain people who somehow transcend their field, and he is one of them.”
When Dr. Clites interviewed to come to UCLA, Dr. SooHoo was among the UCLA Health surgeons with whom he first met. The two began collaborating soon after Dr. Clites arrived. Dr. SooHoo has had the experience of explaining to a patient who has broken their talus bone the difficult choice they face: fusion or amputation of the foot? In many cases, amputation is a better option because function can be restored with a prosthesis. “Still, it’s distressing to amputate an otherwise viable limb,” Dr. SooHoo says. “I asked if there was a way we can save that limb going forward.”
Dr. Clites collaborated with a colleague in the Samueli School, Jonathan Hopkins, PhD, professor of mechanical and aerospace engineering, who was working extensively on compliant devices. Dr. Hopkins came up with several computer-assisted designs, which were 3D printed and tested on cadaveric body parts. “We immediately saw the promise of this,” Dr. SooHoo recalls.
With seed funding from the school of medicine and a $2.5 million New Innovator Award from the National Institutes of Health, they hoped their concept could both save limbs and provide patients with an implant that mimics an external energy-storage-and-return prosthesis — a nuanced, complicated spring that bends and articulates without wearing out.
It is an exciting prospect for patients who otherwise face an excruciating choice. “We really have an opportunity to affect human health in a way that people are rarely able to,” Dr. SooHoo says. “It’s revolutionary, a completely different way of thinking about how we would replace a joint that isn’t working.”
What originated as a device to support a two-inch-long bone in the ankle could have applications across the broad spectrum of the skeleton. “If you look at a hip or knee replacement, they last 15, 20, maybe 25 years. But eventually they are going to fail,” Dr. SooHoo notes. “This device could last 50-to-100 years, longer than a patient’s lifespan. If it works for the ankle and foot, it could potentially be developed as a new form of knee or hip replacement and totally overturn the way we replace all joints.”
“THE PEOPLE LEAST LIKELY TO BE ABLE TO AFFORD THIS CARE ARE THE SAME FOLKS WHO ARE MOST LIKELY TO NEED IT.”
For athletes who are injured or lose a limb, the work Dr. Clites and his surgical colleagues are doing has enormous potential implications. For example, injuries to the ACL, one of the crucial ligaments that support the knee, are not uncommon among athletes participating in many different sports. But because training and injury-prevention paradigms were developed primarily for men, female athletes are at disproportionate risk. In fact, females are two-to-10 times more likely than male athletes to tear their ACL. (The problem was illustrated in the 2023 Women’s World Cup in July when some of the biggest names in the game, and many who were lesser known, were sidelined with ACL injuries.) Such injuries usually don’t heal on their own and require surgery to rebuild the ligament, as well as significant time to rehab the knee.
“But what if we had a prosthesis that we could implant that would prevent the injury from happening in the first place?” asks David R. McAllister, MD, chief of sports medicine.
That is something he and Dr. Clites now are working on together. The aim would be to identify high-risk athletes, such as those undergoing an ACL reconstruction, and implant a small device that would restrict the motion in the knee that causes the injury but not slow down the individual. “It’s a whole different way of thinking about the problem,” says Dr. McAllister, who is head team physician for UCLA Athletics and has been head team physician for the Los Angeles Lakers.
Utilizing the KUKA, he and Dr. Clites have been working with cadaveric knees to better understand the dynamics of the joint’s motion. “If this works in the knee, there’s a good chance it could be applied to other joints,” Dr. McAllister says. He notes that there are approximately 400,000 ACL surgeries each year, mostly suffered by young athletes, and adds that a young person who suffers an ACL tear is at greater risk of developing arthritis in the knee at a young age. “We’re trying to put ourselves out of business,” Dr. McAllister says.
Despite the innovations over the last two decades, there are headwinds to bringing these devices to the commercial market. Research-and-development costs are high, the market is relatively small and it’s difficult to recoup expenditures. What’s more, insurance companies often are unwilling to reimburse patients who want the latest devices.
Providing benefit to injured service members and veterans is, on the other hand, a different story. For the defense department and Department of Veterans Affairs, new developments in prostheses, as well as enhanced surgical techniques for amputation, are of great interest. “Quite frankly, nobody moves standard-of-care faster than the Department of Defense,” Dr. Bernthal says. “If they say this is the care our soldiers should receive, it gets covered very quickly.”
There is optimism in the field of prosthetics, he says. “When I became a doctor nearly 20 years ago, amputation was seen as a failure. Now, when talking to a patient nothing is off limits. You never have to tell someone that the dream they have for their life is not an option. With the prostheses that are available today, and the next generations of prostheses now being developed, they can be fully functional. Someone with a prosthetic limb can run a marathon or compete in an Ironman or get back to active duty in the military.”
And as anatomics continues to evolve, “bionic devices will become more and more integrated with the human body, and with the person’s sense of self,” Dr. Clites says. “Our goal is to transform the field of rehabilitation to improve care, open the door to options and opportunities and, ultimately, enhance the quality of people’s lives.”
Lyndon Stambler is a freelance writer and associate professor of journalism and media studies at Santa Monica College. “Reinventing Extremity Amputation in the Era of Functional Limb Restoration,” Annals of Surgery, February 2021
“Anatomics: Co-Engineering Body and Machine in Pursuit of Synergistic Bionic Performance,” Current Opinion in Biomedical Engineering, August 2023
Featured In
Related Content
Services:
Physicians
Team Member




