April is Minority Health Month, an observance created by the U.S. Department of Health and Human Services Office of Minority Health, to raise awareness to the disproportionate health inequities that persist among racial and ethnic minorities.
This observance was launched in 2001 by the National Minority Health Month Foundation in response to Healthy People 2010, a health-promotion and disease prevention initiative that provides 10-year, measurable public health objectives.
The HHS Office of Minority Health announced this year’s theme as #VaccineReady, to underscore the unequal impacts of the COVID-19 pandemic on racial and ethnic minorities and the importance of ensuring equitable vaccine distribution and acceptance within vulnerable populations.
At UCLA Health, a culturally and linguistically tailored vaccine education series are underway in communities of color to enhance vaccine acceptance.
As more vaccines become available, UCLA Health will remain committed to contributing to the equitable distribution of vaccines to the most socially vulnerable communities.
COVID-19 exacerbated inequities
According to data from the Centers for Disease Control and Prevention, the age-adjusted COVID-19 mortality rate is now higher for American Indian and Alaska Native people than for any other group – and is almost 2 1/2 times the death rate of white and Asian Americans.
Aggregation of data show that Asian Americans represent 4.4% of COVID-related deaths in the U.S., below their population of 5.7%. What this number doesn’t show is that the Asian Americans are highly diverse and are made up of more than 40 distinct ethnicities with myriad cultures, and differences in education level, income, employment, and language. When the data are aggregated, COVID-19 rates are skewed to show that Asian American and Pacific Islander communities fared better than other non-white racial groups.
When the data are disaggregated, the rate of COVID-19 death among Pacific Islanders is 421% higher than for white people in Los Angeles County. Additionally, in California, Filipino Americans account for 35% of COVID-19-related deaths among the Asian population.
Among Latinos in Los Angeles County, the rate of COVID-19 death is 176% higher than white Americans and among Black Americans, it’s 55% higher than white Americans.
The Substance Abuse and Mental Health Services Administration (SAMHSA) referred to COVID-19 and behavioral health disparities as “double jeopardy” for Black and Latino communities.
According to their data, Black and Latino people often have less access to mental health treatment, have treatments end prematurely and experience less culturally informed care. Additionally, Black and Latino people with histories of substance abuse and mental health disorders are more likely to be incarcerated and homeless than the general population – further increasing their risk for COVID-19.
Data from the American Psychiatric Association show that due to limited access to culturally appropriate services and care, Asian Americans may under-report serious psychological distress compared with other racial and ethnic groups and are the least likely of all racial groups to seek mental health services.
Social determinants of health
COVID-19 is just the latest disease to highlight how a history of systemic mechanisms and power structures disadvantage the most vulnerable of these groups. Health inequities among racial and ethnic minorities persisted long before the novel coronavirus arrived.
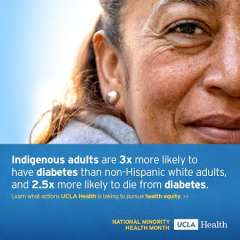
For example, American Indian and Alaska Native adults are three times more likely to have diabetes than white adults, and are 2.5 times more likely to die from complications related to diabetes.
A policy statement from the American Academy of Pediatrics states that American Indian and Alaska Native children and teens are at increased risk of negative health outcomes and are more likely to experience multiple adverse childhood experiences than white children. They have a higher rate of obesity than other children and are more likely to have poor oral health due to limited access to dentists because of lack of recruitment to the Indian Health Services.
The CDC notes that for every 100,000 live births between 2007 and 2016, 17 women died. Black and Indigenous women older than 30 are the most vulnerable, dying at four to five times the rate of their white counterparts. Black women with a college degree are more than five times as likely to die around pregnancy and childbirth than a similarly educated white woman.
What these inequities have in common are the ways in which racism, discrimination, institutional biases and social determinants affect health outcomes. The World Health Organization defines social determinants of health as the conditions in which people are born, grow, live, work and age. These factors are influenced by resource distribution in society.
According to a 2020 study, there are various levels at which social determinants can be addressed – at public policy, community, organizational, interpersonal and individual levels. Across all of these levels, social determinants of health have been aggravated by systemic racism among African American families during the COVID-19 pandemic, the study shows.
To combat this, SAMHSA suggests policy-wide efforts such as data disaggregation, and expanding telehealth and insurance coverage. Additionally, organizations such as health care systems can address inequities through anti-racism action, linguistic and cultural humility, and community-based intervention.
What is UCLA Health doing?
At UCLA Health there are several efforts – internally and externally – that promote greater health and well-being in racial and ethnic minority communities.
Through the Anti-Racism Roadmap, the David Geffen School of Medicine is creating a path to enhance diversity and advance a climate and culture of inclusion throughout the medical school.
In July of 2020, DGSOM launched the Structural Racism & Health Equity Theme that integrates the principles of health equity, anti-racism, and structural social determinants of health throughout the medical school curriculum.
In November, another research theme was launched: the Health Equity and Translational Social Sciences research theme. This joint effort by the UCLA Hospital System and DGSOM aims to gather a multidisciplinary group of scholars to address the challenges of inequity in health.
The UCLA Hospital System Equity Council and the Population Health Equity Committee have been charged with creating, implementing and overseeing health system-wide efforts to advance equitable, patient-centered care and health service access that take into account social and community factors that contribute to health.
Across the health system, several divisions and departments have stood up Equity, Diversity and Inclusion committees and coalitions to address racial and ethnic inequities among patient populations and within their units.
In September 2020, Perinatal Services in the Department of Nursing at UCLA launched the Perinatal Equity, Diversity, & Inclusion Coalition across the David Geffen School of Medicine, ambulatory and inpatient perinatal units at Ronald Reagan and Santa Monica UCLA Medical Centers. The Perinatal EDI Coalition acts to highlight systemic issues to initiate change on local and systemic levels and promote educational programming to bring awareness and culture change to the units and ambulatory areas.
Several coalition members are also active with the California Maternal Quality Care Collaborative QI pilot initiative for Birth Equity. CMQCC conducts research, provides improvement toolkits, and shares data to improve health outcomes for mothers and infants. UCLA Health is one of only a few healthcare institutions participating in this QI pilot with the goal of transforming birth care for Black people in California.
In addition to addressing inequities among racial and ethnic minorities in clinical, research and the medical school settings, here are some other ways UCLA Health is making an impact in the community:
- Held a series of community town halls in English and Spanish to provide information about the COVID-19 vaccine and to optimize vaccine acceptance.
- Venice Family Clinic and UCLA Health delivered nearly 13,000 free meals a week to people experiencing food insecurity in under-resourced communities of color.
- The UCLA Vine Street Clinic recruited racial and ethnic minorities for the Moderna COVID-19 vaccine clinical trial to ensure that the clinical trial participants reflected the diverse populations of our nation.
- UCLA Health Sound Body Sound Mind partnered with the Los Angeles Dodgers Foundation, Lakers Youth Foundation and other community organizations to provide at-home physical education kits for students learning remotely in the Los Angeles, Long Beach and Compton Unified School districts to promote physical activity.
- STOP COVID-19 CA, a coalition addressing gaps in COVID-related misinformation and vaccination accessibility, is leveraging community partnerships to encourage vaccine acceptance in communities of color.
This work is just the beginning. UCLA Health is committed to addressing and mitigating inequities for all racial and ethnic minorities.
To learn more, visit the UCLA Health Office of Health Equity, Diversity and Inclusion, David Geffen School of Medicine Office of Justice, Equity, Diversity and Inclusion, and Anti-Racism Roadmap.



