Picking up a golf club for the first time in 25 years led to an unusual discovery for Jason Daniels.
The Thousand Oaks, Calif., resident was visiting family in Minnesota over the Christmas break last year. He joined his three nephews to play golf at a climate-controlled driving range.
“Naturally, being Uncle Jason, I wasn't going to hold back,” said Daniels, 53. “I was just swinging the club as hard as I could.”
He felt a kink in his neck the night he returned home to California. For the next two months, the project manager for a biotech company could barely move his neck and upper back because of the pain.
A visit to a chiropractor and physical therapy didn’t help. An X-ray was normal. Finally, an orthopedic surgeon ordered an MRI, which showed a swelling on his spinal cord.
Daniels was referred to a neurosurgeon. But when that physician saw the results of the MRI, he cancelled their appointment and advised Daniels to seek other care.
“When a neurosurgeon says, ‘I can't help you, you need to go to a special neurosurgeon,’ it was a little scary,” recalled Daniels.
He was referred again, this time to UCLA Health’s Andrew C. Vivas, MD, the director of adult and pediatric spinal deformity surgery for the neurosurgery department.
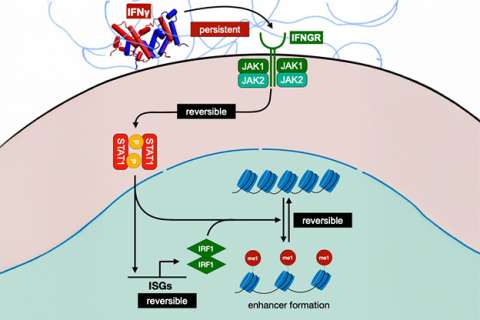
After ordering additional MRIs of Daniels’ entire spine, Dr. Vivas diagnosed him with a rare spinal tumor. The hemangioblastoma, having formed spontaneously, was slowly growing in the blood vessels of the neck’s cervical spine. It was likely benign, and unlike a malignant tumor, wouldn’t move or grow to other areas.
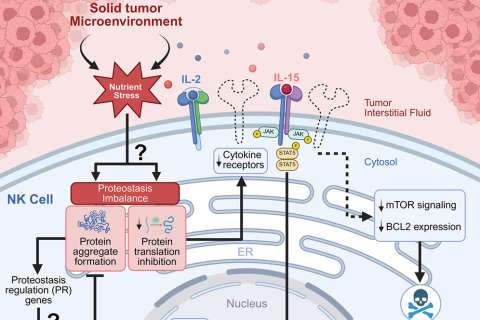
However, the tumor was blocking the flow of spinal fluid, which accumulated and caused a syrinx.
“The spinal cord swells up as if there's a water balloon inside,” said Dr. Vivas, also an assistant professor of neurosurgery, orthopedic surgery and radiation oncology at the David Geffen School of Medicine at UCLA.
During a telehealth visit, Dr. Vivas recommended surgery to remove the tumor.
It was then a few months after Daniels’ overzealous game of golf. The pain was probably from a pinched nerve, a bit of serendipity leading to the discovery of the tumor. But now, his neck felt normal again. Was surgery necessary?
Dr. Vivas explained that the syrinx would likely expand over time and progressively cause paralysis of his arms and legs. The appointment not only convinced Daniels to undergo surgery but also built his trust in the doctor.
“From the time I researched Dr. Vivas to the time I met him, I felt I was in the right hands,” said Daniels. “I thought, I'm just going to go on living my life the way I want to, and then when the time comes for surgery, we'll deal with it.”
Hemangioblastoma surgery
Daniels scheduled the procedure for early August 2025.
The goal was to remove the tumor – but even more important was to protect the spinal cord from injury at the same time, Dr. Vivas said. “Patients walk in. Of course, they want to walk out.”
Key to that is intraoperative spinal monitoring. The technique, first devised at UCLA Health in 1978 by Marc Nuwer, MD, PhD, MS, is now used worldwide, and was found to reduce the rate of paraplegia by 60%.
Before Daniels’ surgery began, fine needles measured the electrical signals that traveled between his brain and arms and legs via the spinal cord. This established a baseline.
As Dr. Vivas began the surgery, a technician in the operating room continuously stimulated Daniels’ nervous system with evoked potentials – tiny pulses of current. Dr. Nuwer assessed the resulting effects, helping Dr. Vivas to proceed safely.
“The goal is to be able to say everything is still at baseline. We haven't seen any adverse changes. In doing so, we reassure the surgeon,” said Dr. Nuwer.
Dr. Vivas moved aside skin and muscles on the back of Daniels’ neck. He made cuts in the bones – the “roof of the spinal canal” – and lifted them off. Next, he opened the dura, the tough outer membrane, to reveal the spinal cord itself. It was a thin tendril of nerves, about the diameter of a thumb.
Sitting right on the whitish-beige surface of the spinal cord was the tumor, orange-colored like a sunset, and about the size of a pea.
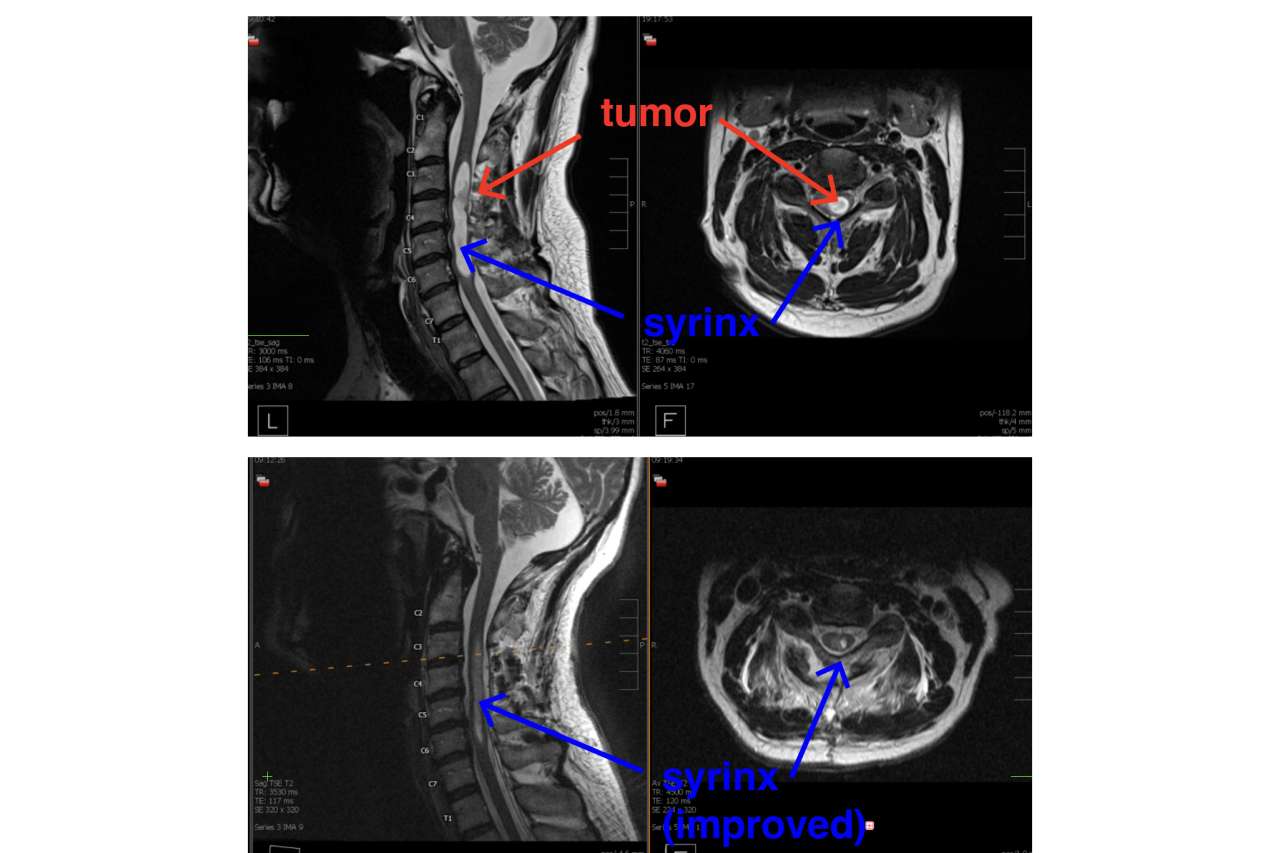
Dr. Vivas examined the nodule under a high-powered surgical microscope. He carefully separated the tumor from the spinal cord, nerve rootlets and any surrounding blood vessels, and lifted it out.
Daniels was groggy after the surgery, but did remember Dr. Vivas telling him, “Jason, we've got it all, you're good.”
Daniels recovered in the hospital for two days. The day after surgery, he was walking along the hallway outside his hospital room. Though he was stiff and sore, he said he didn’t feel much pain.
About a week later, just as Daniels was returning to work part-time, the pathology report confirmed the tumor was benign.
Multidisciplinary collaboration
A few weeks after his spinal tumor was removed, Daniels was back to his regular routine of morning workouts and weekend hikes with his dog, Abby.
He plans to write a letter of thanks to his care team at UCLA Health.
“I felt like a rock star the moment I arrived there,” said Daniels. “From the valet attendant to the person ordering my lunch to the nurse who wheeled me out, everybody just treated me so professionally. I'm forever grateful. When you get to receive that care firsthand, it's pretty amazing.”
That is a result, Dr. Vivas said, of the “team-based, multidisciplinary approach” at the medical center.
“I can't do the work that I do without all of the other people that are part of this team,” said Dr. Vivas. “And that team extends even into the community. His original orthopedic surgeon and neurosurgeon correctly diagnosed him and said, ‘We're going to get you to a place that does a really good job with this.’
“And that speaks to the incredible working relationship that UCLA Health has with the community of medical physicians as well.”