Chronic back and lower extremity pain are leading causes of disability worldwide, significantly impacting the quality of life and productivity of the patients affected by them. For these patients, spinal cord stimulation (SCS) — a non-pharmacological, neurostimulation treatment that involves the surgical implantation of electrodes and a power source to deliver electrical current to the spinal cord to reduce pain signals to the brain — offers an advanced, safe and minimally invasive treatment option.
SCS is not a new medical technology, but has evolved considerably since its introduction in the 1960s. “It was historically used for patients who had undergone spine surgery but continued to experience pain,” explains Jonathan Droessler, MD, a specialist in interventional physiatry at UCLA’s Department of Orthopaedic Surgery.
“Today, it’s used for patients with intractable pain lasting more than six months.”
Expanding applications
Over the years, SCS has become one of the most commonly prescribed treatments for patients experiencing intractable pain even after six months or more of conventional medical management.
In addition to chronic postoperative pain, it’s used to treat complex regional pain syndrome, a condition in which the sympathetic nervous system causes severe pain and inflammation – usually in an arm or a leg – often as the result of an injury, stroke or heart attack. It is also beneficial for patients with phantom limb pain following amputation.
“Recently, the scope of patients that can be helped with SCS has also expanded,” says Dr. Droessler.
Since 2023, the U.S. Food and Drug Administration has approved SCS systems for treating painful diabetic peripheral neuropathy, which causes pain, numbness and burning sensations in the limbs of patients with diabetes – a huge patient population in the United States.
“It has also been approved for patients with chronic back pain who want to avoid surgery.”
Selecting the right patients
Not all patients are candidates for SCS, and proper patient selection is crucial for successful outcomes. In addition to patients with chronic radicular pain, SCS can be an effective tool for patients with axial pain who are not candidates for surgery, and patients with failed back surgery.
SCS is often recommended for patients who have tried everything else and continue to struggle with their spine health.
“The ideal candidates are those who have exhausted conservative treatments such as physical therapy, chiropractic care, acupuncture, injections or even surgery, and still experience significant pain that limits their daily activities,” Dr. Droessler says.
“These are often the patients who say, ‘I’ve tried everything, and I don’t want to rely on medication anymore.’”
Contraindications include active infections, untreated substance abuse issues and certain medical conditions that increase surgical risk. All patients undergo a psychological evaluation to ensure they are prepared for the treatment process.
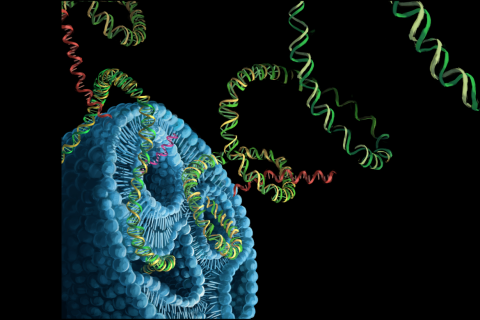
How spinal cord stimulation works
SCS uses an implantable device that delivers electrical currents to the spinal cord to disrupt pain signals.
The process begins with a trial phase that lasts about a week, during which a temporary device is inserted into the spine and connected to an external transmitter. Throughout the trial period, the patient tests different stimulation settings to evaluate the device’s effectiveness.
“We’re looking for more than 50% improvement in function or pain reduction during the trial,” Dr. Droessler says. “Most patients report significant improvements, allowing them to return to activities they couldn’t do before.”
If the trial is successful, patients proceed to a second outpatient procedure in which the device is implanted underneath the skin and the trial electrodes are replaced with permanent electrodes. Recovery typically lasts four to eight weeks, during which patients gradually increase physical activity.
Advances in SCS technology
Innovations in SCS technology have made the treatment more effective and comfortable. “The miniaturization of batteries has been a game-changer,” notes Dr. Droessler. “Smaller batteries reduce discomfort, making the implantation process more tolerable for patients.”
Advances in software, such as closed-loop systems, represent another leap forward. Unlike traditional systems, closed-loop devices monitor spinal cord responses in real time and adjust stimulation accordingly. This prevents “zingers,” or uncomfortable jolts that can occur during movement, improving the experience for active patients.
Evidence of effectiveness
A recent study published by JAMA Network found that SCS is associated with greater improvements in pain and function compared with conventional medical management. While long-term success rates depend on proper patient selection, advances in technology are steadily enabling improved outcomes.
Dr. Droessler emphasizes the importance of close collaboration with referring physicians. “Primary care doctors, surgeons, endocrinologists and podiatrists play a key role in identifying patients who could benefit from SCS,” he says. “We work with them to ensure patients are well-informed and prepared for the process.”
For patients grappling with chronic pain, SCS offers hope when other treatments fall short. “It’s not for everyone, but for the right patients, SCS can be life-changing,” says Dr. Droessler.