When Jamil Newirth was 32, doctors told him he had terminal brain cancer and about 17 months to live. Today, at 45, the Hawaii native is thriving — thanks to a groundbreaking glioblastoma vaccine developed at UCLA
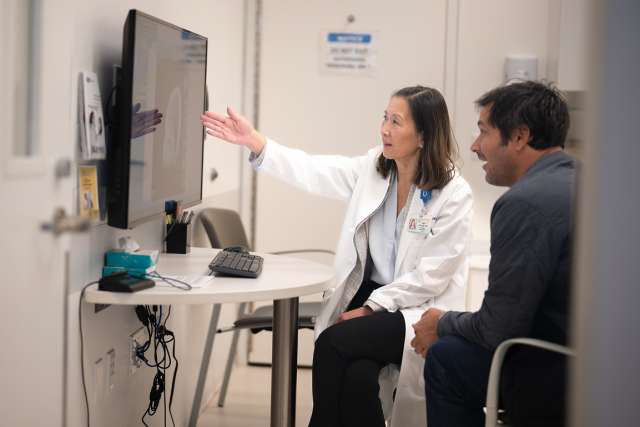
Dr. Liau, chair of the neurosurgery department at the David Geffen School of Medicine at UCLA and director of UCLA’s NCI-funded Brain Tumor SPORE (Specialized Program of Oncologic Research Excellence), has spent decades turning the immune system into a weapon against brain tumors. Supported in part by the National Institutes of Health, her research led to the development of DCVax-L, a personalized vaccine that has given new hope to patients facing a devastating diagnosis.
The science behind the vaccine is surprisingly elegant. Liau and her team found that by taking a patient’s own immune cells, exposing them in the lab to pieces of that person’s glioblastoma tumor, and then injecting them back into the patient, the immune system could be “taught” to recognize and attack the cancer. Over a series of clinical trials, DCVax-L was shown to help extend the lives of people with newly diagnosed and recurrent glioblastoma — with some surviving far beyond the expected two-year expected survival for this diagnosis.
DCVax-L potentially represents one of the first successful brain cancer vaccines and a milestone in the field of cancer immunotherapy.
While Dr. Liau’s work trains the immune system to fight back, Dr. Aparna Bhaduri, an assistant professor of medicine and biological chemistry and member of the UCLA Broad Stem Cell Research Center, is using stem cell technology to uncover how glioblastoma grows, adapts and resists treatment. Her lab builds 3D tumor-immune organoid models — miniature, stem cell-derived brain tissues implanted with patient tumor samples — to recreate and study the complexity of the human brain and its tumor environment.
These all-human models allow Dr. Bhaduri’s team to observe how tumor, brain and immune cells interact in real time, revealing how glioblastoma communicates with its surroundings and evolves to evade treatment. The system closely mirrors the complexity of the human brain — something that traditional mouse models can’t fully capture — giving researchers a clearer picture of what drives tumor growth and why many current therapies fall short.
Dr. Bhaduri’s group is using this platform to test combinations of existing drugs and identify strategies that could more effectively target the diverse cell populations within a tumor. The ultimate goal, she says, is to lay the groundwork for more personalized and effective treatments for glioblastoma.
“We now have tools that let us study the human brain’s complexity and how cancer exploits it in ways we couldn’t before,” Dr. Bhaduri says. “That’s what makes this work so exciting — it moves us closer to understanding how these tumors behave and how we can finally change the outcome for patients.”
Related articles
UCLA discovers first stroke rehabilitation drug to repair brain damage in mice
Read more about UCLA’s latest research advancements to combat brain cancer