Thoracic Outlet Syndrome
Find your care
Our thoracic surgeons provide a full range of services with outcomes that are among the best in the country. To learn more,
call 310-267-9099.
Thoracic Outlet Syndrome FAQ
What is the Thoracic Outlet?
The thoracic outlet is the region of the body between the neck and the chest. It is an important area because the main nerves of the arm, the brachial plexus, run through this region after they come out of the spinal cord. Additionally, the main arteries and veins that carry blood to and from the arm, the subclavian artery and vein, also run through this area.

What is Thoracic Outlet Syndrome?
Thoracic Outlet Syndrome, or TOS, is actually a trio of three syndromes- neurogenic TOS, venous TOS, and arterial TOS.
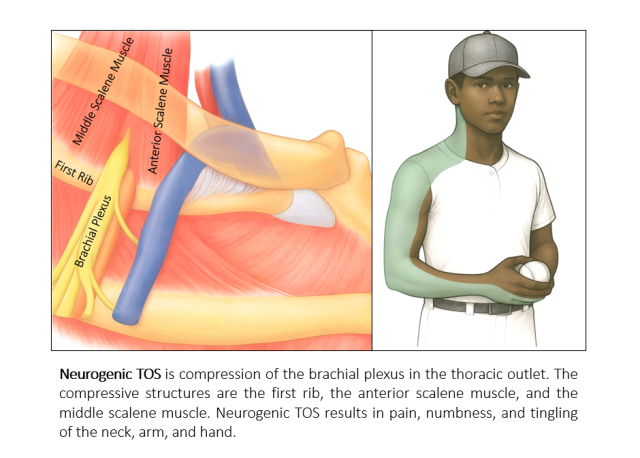
Neurogenic TOS is the most common form of TOS. In neurogenic TOS, the brachial plexus is compressed by its surrounding structures in the thoracic outlet. These compressive structures are the first rib, the anterior scalene muscle, and the middle scalene muscle. Compression of the brachial plexus in the thoracic outlet causes pain in the front of the neck which tends to radiate down the inner portion of the arm into hand and fingers, and that can also spread to the head and back. The brachial plexus runs through a tunnel between the first rib and scalene muscles, and this tunnel naturally becomes narrow with the hand above the head. Consequently, lifting the arm tends to worsen the symptoms of neurogenic thoracic outlet syndrome.
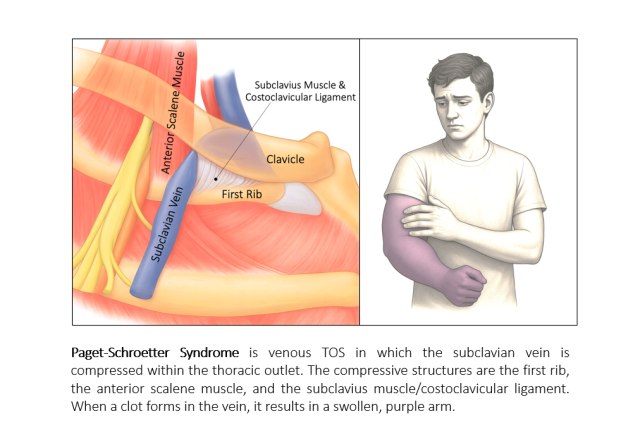
Venous TOS is the next most common form of TOS. In venous TOS, the subclavian vein is compressed by its surrounding structures in the thoracic outlet. These compressive structures are the first rib, the anterior scalene muscle and the subclavius muscle/costoclavicular ligament. Compression of the subclavian vein can cause inflammation inside of the vein that can result a blood clot to form and swelling and purple color changes of the arm. When there is a blood clot this is also known as Paget-Schroetter Syndrome. There is another rarer form of Venous TOS called McCleery Syndrome in which there is no clot in the vein but patients can have intermittent swelling and color changes of the arm.
- Arterial TOS is a very rare form of TOS in which the subclavian artery is compressed in the thoracic outlet on its way to the arm. The structures that compress the subclavian artery are similar to those that compress the brachial plexus in neurogenic TOS because the subclavian artery and the brachial plexus run together. These structures are the first rib, the anterior scalene muscle, and the middle scalene muscle. The symptoms of arterial TOS affect the arm and hand and included paleness, coolness, weakness, and pain.
What is the cause of Thoracic Outlet Syndrome?
TOS is thought to occur from different kinds of injury to the structures in the thoracic outlet in patients who have a naturally smaller thoracic outlet. TOS is common in patients with who have had an accident or fall that could affect the muscles of the thoracic outlet or the first rib. Thes same structures can also be affected by repetitive injury from overuse of the arm. For example, TOS is common in athletes that commonly perform hand-over-head activities, including pitchers, swimmers, basketball and volleyball players, and others. It is also common in workers who commonly lift their arms including painters, electricians, and others. It is also seen in avid computer users.
One to ten percent of patients with neurogenic TOS have a cervical rib that can contribute to compression in the thoracic outlet. A cervical rib is an extra rib at the bottom of the neck right above the first rib. Most of the time this is an incomplete rib. The cervical rib itself and the scalene muscle attachments to the cervical rib can cause compression of the brachial plexus and the subclavian artery. A cervical rib is in common in patients with the rare arterial form of TOS.

How is Thoracic Outlet Syndrome diagnosed?
Neurogenic TOS. Neurogenic TOS is difficult to diagnose because its symptoms can be the same as symptoms of other conditions of nerve compression in the neck and arm including cervical disc compression on the spinal cord, ulnar nerve entrapment, and carpal tunnel syndrome. Shoulder problems and general pain conditions can also appear like neurogenic TOS. There is also no test that can definitively diagnose neurogenic TOS. Consequently, it is important that patients suspected to have neurogenic TOS be evaluated by a TOS expert.
The Society of Vascular Surgeons has published expert guidelines to help providers diagnose patients with neurogenic TOS. According to these guidelines, the diagnosis of neurogenic TOS is supported by a history and physical exam that are consistent with this syndrome, a lack of other conditions that explain the symptoms, and a positive response to a scalene muscle block.
Scalene muscle block is a test in which the anterior scalene muscle is injected with lidocaine to temporarily relaxes the scalene muscle and its compression on the brachial plexus. If the patients’ symptoms improve after this block, this is highly supportive of the diagnosis of neurogenic TOS.

MRI of the cervical spine and EMG tests may be recommended to investigate the presence of other nerve compression disorders. A chest or neck x-ray should be performed to investigate whether there is a cervical rib. MRI of the brachial plexus may be recommended to better understand the anatomy of the thoracic outlet.
To understand the severity of your disease and its impact on your life, your provider may ask you to fill at a questionnaire at several points in your journey.
Venous TOS. Patients with Paget-Schroetter Syndrome develop a clot in the subclavian vein and experience rapid onset of arm swelling and purple color changes of the arm. Ultrasound of the subclavian vein will demonstrate a clot within the vein, and this can be confirmed on venogram. If the patient has not had any prior procedures on this vein, it is very likely that they have venous TOS. In patients with symptoms of venous TOS and no clot in the subclavian vein, a venous ultrasound with the arm up and down is useful to investigate the dynamic narrowing that can be seen in venous TOS without a clot (McCleery Syndrome).
Arterial TOS. Patients with arterial TOS have signs on physical exam that include paleness, coolness, and weakness of the arm and hand. An ultrasound of the subclavian artery will show narrowing and sometimes clot in the artery and this will be confirmed by arteriogram.
How is Thoracic Outlet Syndrome treated?
Neurogenic TOS. Patients diagnosed to with neurogenic TOS will undergo physical therapy to loosen the muscular compression on the brachial plexus, to strengthen stabilizing muscles, and to correct posture, all of which can improve the musculoskeletal framework of the thoracic outlet to results in less compression. If patients do not experience a meaningful improvement in their symptoms, surgery for TOS may be offered.
Venous TOS. Patients with Paget-Schroetter Syndrome have a clot in their subclavian vein. There are typically 3 phases of treatment. In the first phase, the clot is removed using endovascular methods. This includes a venogram in which a catheter is placed into a lower arm vein and dye is injected to first show the location and features of the clot. Though this catheter, special instruments to perform a thrombectomy procedure in which this is removed. The patients are placed on blood thinner medications to temporarily keep the clot from reforming. Phase 2 begins about 3-4 weeks afterwards when surgery is performed to remove the first rib and surrounding muscles that are compressing the vein to permanently keep the clot from reforming. The patients are kept on their blood thinner medications. Phase 3 occurs about 3-4 weeks after thrombectomy at which time the subclavian vein is re-evaluated with either ultrasound or venogram. At this time, about half of patients will require and endovascular dilation of the vein to address leftover narrowing that can result from the initial disease.
Arterial TOS. Patients with arterial TOS are treated with surgery to remove the first rib and scalene muscles that are compressing the artery. In some cases, a section of the artery may need to be repaired or replaced. Blood thinner medications are also used.
What is the surgical treatment for TOS?
The surgical treatment for TOS is first rib resection and scalenectomy. This operation removes the structures that are compressive on the brachial plexus, subclavian vein, and subclavian artery. In neurogenic and arterial TOS, this operation removes the first rib, anterior scalene muscle, and middle scalene muscle. In venous TOS, the subclavius muscle and costoclavicular ligament are also removed. During these procedures, it is common to find scar tissue surrounding the brachial plexus and/or subclavian artery and vein. Removal of this scar tissue is also performed in procedures called brachial plexus neurolysis and external venolysis.
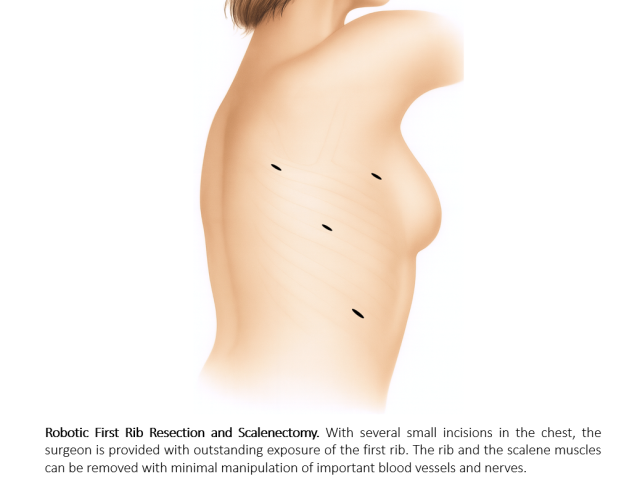
There are several approaches to first rib resection and scalenectomy procedures. Traditional approaches included incisions above the collarbone (supraclavicular) and in the armpit (transaxillary). A newer approach is called robotic first rib resection and scalenectomy. This approach provides the surgeon improved visualization and exposure of the first rib and allows the operation to be conducted without manipulating or stretching important nerves including the brachial plexus and phrenic nerve, and important arteries including the subclavian artery. The robotic approach is performed by 4 small incisions on the chest and patients commonly are discharged home the following day.