Gigantism
Find your care
We treat pituitary tumors using the latest innovations in minimally invasive procedures. To connect with an expert in the pituitary tumor program, call 310-825-5111.
Gigantism is a serious condition that is nearly always caused by an adenoma, a tumor of the pituitary gland. Gigantism occurs in patients who had excessive growth hormone in childhood. The pituitary tumor cells secrete too much growth hormone (GH), leading to many changes in the body.
Gigantism: Expert Care in Southern California

The physicians at the UCLA Pituitary Tumor Program offer comprehensive management of gigantism. Our years of experience in diagnosing, treating and managing pituitary conditions, as well as the high volume of patients we see every year, make us one of the best pituitary programs in the United States.
Learn more about gigantism:
Gigantism: Physiology
Gigantism usually presents in childhood or young adulthood. If a pituitary tumor that secretes growth hormone develops after the bone growth plates fuse, the result is acromegaly.
Gigantism is a form of familial pituitary adenomas, and may run in some families due to a genetic mutation.
Gigantism can also be associated with other conditions, including:
- Carney complex
- McCune-Albright syndrome (MAS)
- Multiple endocrine neoplasia type 1 (MEN-1)
- Neurofibromatosis
Normal Growth Hormone Physiology
- Growth hormone is secreted by the pituitary gland in a pulsatile fashion, meaning that its level goes up and down significantly throughout the day.
- For this reason, growth hormone measured at a random time of the day may be meaningless for diagnosis
- Growth hormone release normally falls dramatically after eating a large quantity of sugar, a phenomenon that is useful in making the diagnosis in acromegaly because tumor cells do not exhibit this response (see oral glucose tolerance test)
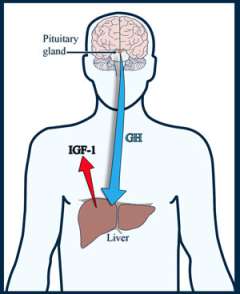
- Growth hormone has direct effects on the body, but like most pituitary hormones, acts on other specialized gland cells in the body to stimulate the release of another hormone
- Growth hormone acts on special cells in the liver, leading to the release into the blood stream a hormone called Insulin-like Growth Factor (IGF-1).
- IGF-1 is also called Somatomedin-C
- Because IGF-1 is released in a more steady fashion, its levels do not go up and down quickly and therefore it is a better hormone to measure to screen for acromegaly
- Growth hormone acts on special cells in the liver, leading to the release into the blood stream a hormone called Insulin-like Growth Factor (IGF-1).
Normal Control of Growth Hormone Production
A part of the brain called the hypothalamus controls the amount of growth hormone production by sending chemicals ("neuropeptides") down the pituitary stalk to the pituitary gland.
- The main neuropeptide that stimulates growth hormone release is called growth hormone releasing hormone (GHRH).
- The main neuropeptide that inhibits growth hormone release is called somatostatin; drugs that mimic the effects of somatostatin (somatostatin analogs, or SSA's) are used to treat acromegaly.
Gigantism: Symptoms
The main symptom associated with gigantism is large body stature with increased height compared to peers. Muscles and organs may be enlarged as well.
Other gigantism symptoms include:
- Delay in puberty
-

Physical changes similar to patients with acromegaly, including:
- Abnormal enlargement of the hands and feet
- Widening of distal fingers and toes, called "paddle" toes
- Hands feel like soft bread dough
- Changes in facial features, which can be quite prominent:
- Enlarged forehead and jaw
- Pronounced underbite
- Spreading teeth
- Enlarged tongue, nose and lips
- Deepening of the voice in males
- Skin changes:
- Increased number of skin tags
- Oily skin and excessive sweating
- Increased tissue in the wrists can lead to nerve compression, which may cause carpal tunnel syndrome
- Arthritis
- Headache
Serious conditions related to long-standing, untreated gigantism/acromegaly include
- High blood pressure
- Diabetes mellitus (adult-onset or Type 2)
- Heart disease, including heart failure due to heart enlargement
Giants are at increased risk of developing other tumors or lesions of the body:
- Thyroid cancer occurs at a higher frequency; talk to your doctor about screening
- You should also undergo regular colonoscopies to screen for colon polyps
Gigantism: Macroadenomas
Macroadenomas are large pituitary tumors. Large tumors can compress surrounding structures, primarily the normal pituitary gland and optic (visual) pathways, causing symptoms. The symptoms that result from the compression are independent of the effects of excess growth hormone secretion. Macroadenomas can cause:
-

Vision loss. This occurs when macroadenomas grow upward into the brain cavity, compressing the optic chiasm.
- A loss of the outer peripheral vision, called a bitemporal hemianopsia
- When severe, a patient can only see what is directly in front of them
- Many patients do not become aware of their visual loss until it is quite severe
- Other visual problems can include:
- Loss of visual acuity (blurry vision), especially if the macroadenoma grows forward and compresses an optic nerve.
- Colors not perceived as bright as usual
Pituitary Failure or Hypopituitarism
Increased compression of the normal gland can cause hormone insufficiency, called hypopituitarism. The symptoms depend upon which hormone is involved.
- Reduction of sex hormones, luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
- In men, this can lead to a low testosterone level, causing decreased sexual drive and impotence.
- In some cases, there can be loss of body and facial hair.
- In women, this can lead to infertility.
- Large pituitary tumors can slightly elevate blood prolactin levels. Doctors think this occurs because of compression of the pituitary stalk, the connection between the brain and the pituitary gland. It is called the "stalk effect."
- In premenopausal women, this can lead to reduction or loss of menstrual periods and/or breast milk production (galactorrhea).
- Prolactin levels are only slightly elevated, as opposed to prolactinomas in which the prolactin level is usually very high.
More severe hypopituitarism can lead to hypothyroidism or abnormally low cortisol levels, which may be life threatening. Symptoms of severe hypopituitarism include:
- Loss of appetite
- Weight loss or weight gain
- Fatigue
- Decreased energy
- Decreased mental function
- Dizziness
Changes in hormonal function can cause electrolyte imbalance in the blood, typically low sodium levels (hyponatremia). Symptoms could include:
- Fatigue
- Seizures
Gigantism: Diagnosis
Your doctor will conduct a physical examination and ask you about your medical history and symptoms.

Other diagnostic procedures include:
Hormone Testing for Gigantism
Doctors are looking for an elevated blood IGF-1 level to diagnose gigantism.
Your doctor may order an oral glucose tolerance test (OGTT) to confirm the diagnosis.
-

Drinking 75 grams of glucose solution lowers blood GH levels to less than one nanogram per milliliter (ng/ml) in healthy people.
- In acromegalics, this suppression does not occur. In fact, sometimes GH levels increase.
Learn more about hormone testing at the UCLA Pituitary Tumor Program.
MRI Imaging
One method we use for detecting pituitary tumors is using sophisticated magnetic resonance imaging (MRI) of the pituitary gland. At the Pituitary Tumor Program, we use a special MRI pituitary protocol in order to best visualize the tumor. The vast majority (90%) of GH-secreting tumors are macroadenomas.
Treatment for Gigantism
The optimal treatment of gigantism depends on multiple factors, including:
- Size and location of the tumor; invasive tumors may not be able to be cured surgically
- Your age and medical condition
Typically, more than one specialist is involved in the management of pituitary adenomas. At the Pituitary Tumor Program, your medical team includes a special endocrinologist called a neuro-endocrinologist who has specific expertise in the treatment of acromegaly and gigantism.
Surgery for Gigantism

Surgically removing the selected tumors offers the best chance for cure. You should seek the care of an experienced neurosurgeon that performs a high volume of pituitary surgeries every year. Our neurosurgeons practice the latest surgical techniques, such as the expanded, endoscopic endonasal approach, allowing us to cure pituitary tumors that were previously deemed unresectable (unable to be removed surgically).
The success of the surgery depends on a number of factors:
- Tumors that have invaded beyond the confines of the sella (the space where the normal pituitary gland sits) have a lower chance of cure surgically.
- The first surgery offers the greatest chance of cure; the cure rate with a second or third surgery is much lower.
Long-term cure rates after transsphenoidal (pituitary tumor) surgery:
- 80 percent to 85 percent or patients with smaller tumors (microadenomas)
- 50 percent to 60 percent of patients with larger tumors (macroadenomas)

Medical Therapy for Gigantism
The medical treatment for gigantism/acromegaly is improving, and in some cases, doctors use medication instead of surgery, as the first course of treatment. However, both medical and surgical therapies may be required to control acromegaly.
Medications include:
- Somatostatin analog (Octreotide, Lanreotide) injections, typically administered on a monthly basis, suppress growth hormone production in about 70 percent of patients.
- Significant tumor shrinkage occurs in 30 to 50 percent of patients.
- Injections often improve symptoms of soft tissue swelling, headache, joint pains and sleep apnea.
- Patients require lifelong treatment with somatostatin.
- Drugs that block the action of growth hormone on liver cells, such as a daily injection of Pegvisomant. When effective, IGF-1 levels can normalize, but elevated growth hormones remain.
- Drugs that mimic the effect of dopamine, such as cabergoline, are effective in a small number of patients. These medications are the same ones used to treat prolactinomas.
The UCLA Pituitary Tumor Program has clinical trials testing newer medications for the treatment of acromegaly and gigantism.

Gigantism Treatment: Radiation Therapy
For some patients, surgery or medication is not sufficient to control the acromegaly. In these cases, doctors may recommend stereotactic radiosurgery. Stereotactic radiosurgery is a technique in which doctors aim a highly focused dose of radiation to the tumor. It takes an average of 18 months to lower the GH and IGF-1 levels.
The radiation beam is designed to target only the tumor. The surrounding brain structures receive only a fraction of the radiation dose and are typically unharmed, with the exception of the normal pituitary gland. In children, though, radiation therapy may cause learning disabilities, obesity and emotional changes, so doctors may limit radiation use to situations when all other treatment options have failed.
A consequence of radiation treatment is that it can cause delayed pituitary failure. This typically occurs several years after treatment, and therefore continued long-term follow-up with an endocrinologist is important. Hormone replacement may be required.
Contact Us
To schedule an appointment with one of our physicians at the Pituitary Tumor Program, please call (310) 825 5111.